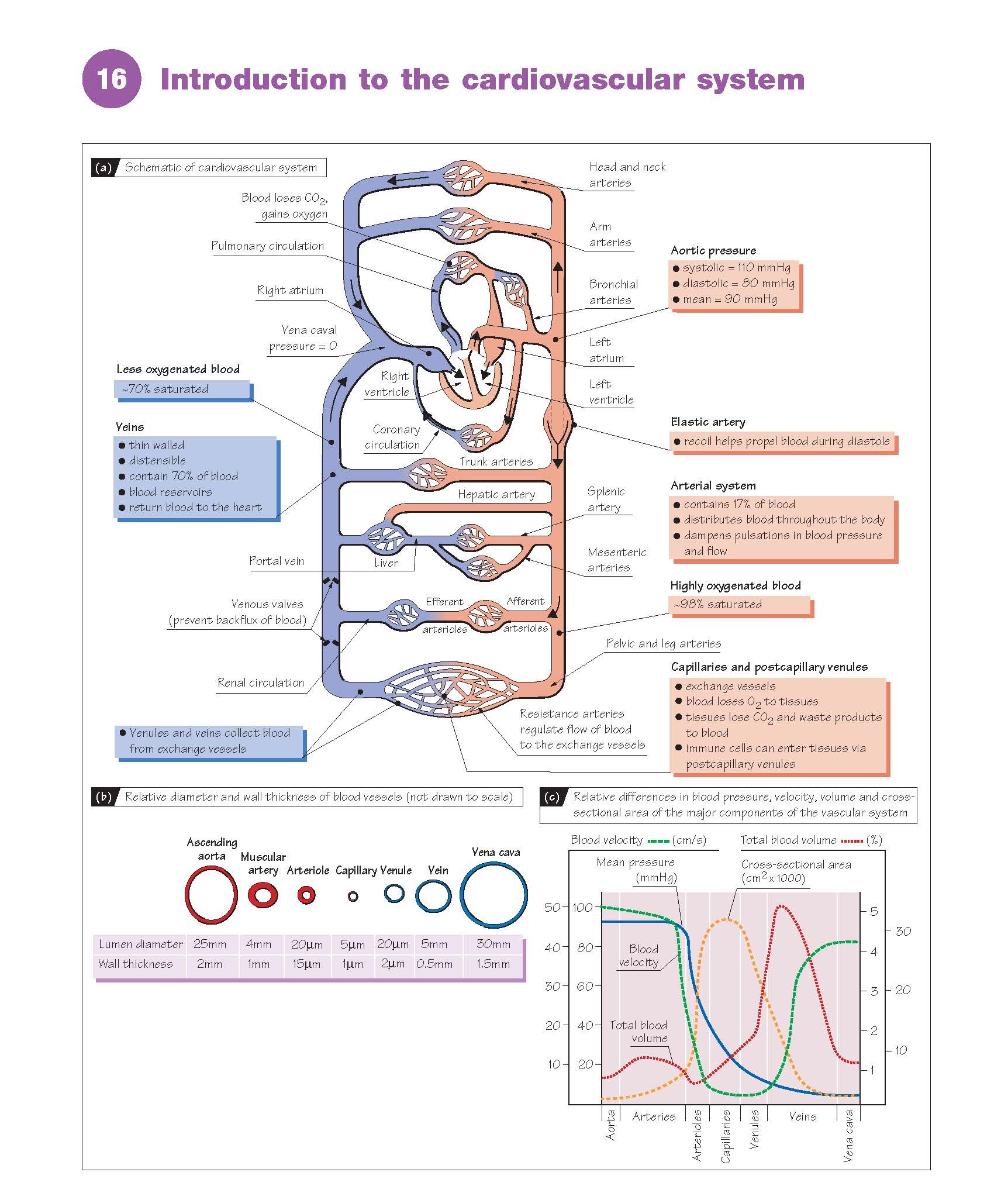
Introduction to The Cardiovascular System.
The cardiovascular system comprises the heart
and blood vessels, and contains ∼5.5 L of
blood in a 70 g man. Its main functions are to distribute O2 and
nutrients to tissues, transfer metabolites and CO2 to excretory organs and the
lungs, and transport hormones and components of the immune system. It is also
important for thermoregulation. The cardiovascular system is arranged mostly in
parallel, i.e. each tissue derives blood directly from the aorta (Fig.
16a). This allows all tissues to receive fully oxygenated blood, and flow can
be controlled independently in each tissue against a constant pressure head by
altering the resistance of small arteries (i.e. arteriolar constriction or
dilatation). The right heart, lungs and left heart are arranged in series.
Portal systems are also arranged in series, where blood is used to transport
materials directly from one tissue to another, such as the hepatic portal
system between digestive organs and the liver. The function of the
cardiovascular system is modulated by the autonomic nervous system (Chapter 7).
Blood vessels
The vascular system consists of arteries
and arterioles that take blood from the heart to the tissues,
thin-walled capillaries that allow the diffusion of gases and
metabolites, and venules and veins that return blood to the
heart. The blood pressure, vessel diameter and wall thickness vary throughout
the circulation (Fig. 16b,c). Varying amounts of smooth muscle are
contained within the vessel walls, allowing them to constrict and alter their
resistance to flow (Chapters 11 and 21). Capillaries contain no smooth muscle.
The inner surface of all blood vessels is lined with a thin monolayer of endothelial
cells, important for vascular function (Chapter 21). Large arteries are elastic
and partially damp out oscillations in pressure produced by the pumping of
the heart; stiff arteries (age, atherosclerosis) result in larger oscillations.
Small arteries contain relatively more muscle and are responsible for
controlling tissue blood flow. Veins have a larger diameter than equivalent
arteries, and provide less resistance. They have thin, distensible walls and
contain ∼70% of the total blood volume (Fig. 16c).
Large veins are known as capacitance
vessels and act as a blood volume reservoir; when
required, they can constrict and increase the effective blood volume (Chapter
21). Large veins in the limbs contain one-way valves, so that when
muscle activity (e.g. walking) intermittently compresses these veins they act
as a pump, and assist the return of blood to the heart (the muscle pump).
The heart
The heart is a
four-chambered muscular pump which propels blood around the circulation. It has
an intrinsic pacemaker and requires no nervous input to beat normally, although
it is modulated by the autonomic nervous system (Chapter 7). The volume
of blood pumped per minute (cardiac
output) is ∼5 L at rest in humans, although this can increase to above 20 L during exercise. The volume ejected per beat
(stroke volume) is ∼70 mL at
rest. The ventricles perform the work of pumping; atria assist
ventricular filling. Unidirectional flow through the heart is maintained by valves between the chambers and
outflow tracts. Contraction of the
heart is called systole (pronounced sis′-to- ley) ; the
period between each systole, when the heart refills with blood, is called diastole
(di-as′-to-ley).
The systemic circulation
During systole,
the pressure in the left
ventricle increases to ∼120 mmHg, and blood is ejected into the aorta.
The rise in pressure stretches the elastic walls of the aorta and large
arteries, and drives blood flow. Systolic pressure is the maximum
arterial pressure during systole (∼110 mmHg). During diastole, arterial blood flow
is partly maintained by elastic recoil of the walls of large arteries. The
minimum pressure reached before the next systole is the diastolic pressure (∼80 mmHg).
The difference between the systolic and diastolic pressures is the pulse
pressure. Blood pressure is expressed as the systolic/diastolic arterial
pressure, e.g. 110/80 mmHg. The mean blood pressure (mean arterial
pressure, MAP) cannot be calculated by averaging these pressures, because for
∼60% of
the time the heart is in diastole. It is instead estimated as the diastolic
pressure plus one-third of the pulse pressure, e.g. 80 + 1/3(110 − 80) ≈ 90
mmHg.
The major arteries divide
repeatedly into smaller muscular arteries, the smallest of which
(diameter <100 μm) are called arterioles. Tissue blood flow is
regulated by the constriction of these small arteries, referred to as resistance
vessels. The mean blood pressure at the start of the arterioles is ∼65 mmHg.
The arterioles divide into dense networks of capillaries in the tissues,
and these rejoin into small and then larger venules, the smallest veins.
Capillaries and small venules provide the exchange surface between blood and
tissues, contain no smooth muscle and are called exchange vessels; some
gas exchange also occurs across the walls of small arterioles. The pressure on
the arterial side of capillaries is ∼25 mmHg and, on the venous side, ∼15 mmHg. Venules converge
into veins and finally the vena
cava. This returns the partially
deoxygenated and CO2- loaded blood to the right atrium. The pressure
in the vena cava at the level of the heart is called the central venous
pressure (CVP), and is close to 0 mmHg.
The pulmonary circulation
The right atrium helps to fill the
right ventricle, which pumps blood into the pulmonary artery and lungs.
The pulmonary circulation is shorter than the systemic, and has a lower
resistance to flow. Less pressure is therefore required to drive blood through
the lungs; the pulmonary artery
pressure is ∼20/15 mmHg. Gas exchange occurs in capillaries surrounding the alveoli (small air sacs) of the lungs. These
rejoin to form pulmonary venules and
veins, and oxygenated blood is returned through the pulmonary vein to the left
atrium, and hence to the left ventricle. The metabolic requirements of the
lungs are not met by the pulmonary circulation, but by the separate bronchial
circulation, the venous outflow of which returns to the left side of the
heart (Fig. 16a).