Histologic and Cytologic Diagnosis
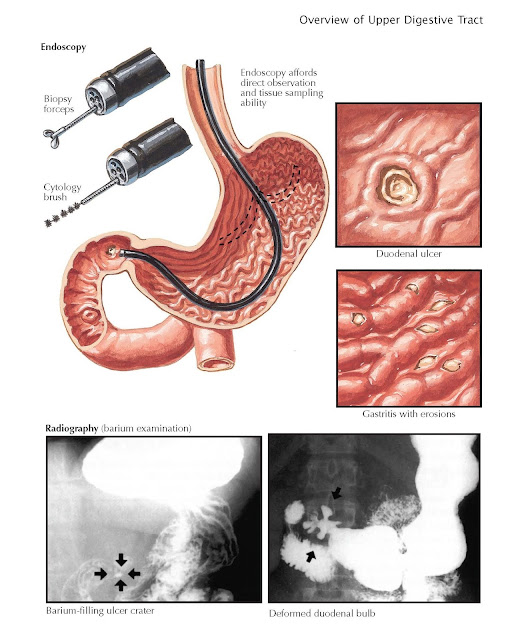
Safe, minimally invasive techniques have been developed to definitively
diagnose most digestive disorders, including the acquisition of cytologic or
histologic specimens. This has been particularly important in malignant
disease, where it is rarely, if ever, acceptable to consider treatment without
first making a “tissue diagnosis.” In many more cases, cytology or pathology
obtained by endoscopy can exclude a malignancy or diagnose a malignancy that
does not require surgical intervention (e.g., gastric mucosa-associated
lymphoid tissue [MALT] lymphomas, which are treated with antibiotics;
malignancies that are diffusely metastatic and therefore beyond the benefit of
surgery).
In many situations, highly accurate
photo documentation may be a most valuable tool in making the diagnosis and
guiding therapy. Much more often, however, biopsies are essential, even at
times when the gross appearance is normal. Common examples of this in the upper
gastrointestinal tract include eosinophilic esophagitis and celiac disease.
Histology can also determine the cause of what may appear to be mild
nonspecific erythema to reveal that it is due to an infection or Crohn disease.
Histologic specimens obtained by endoscopic biopsies or cytologic specimens
provided by brushes or fine-needle aspiration provide the clinician with definitive
data with which an effective therapeutic strategy can be designed.
When receiving the results of a
procedure, the ordering clinician should clarify whether biopsies or cytologic
specimens were taken and the number of specimens taken. Providing the
pathologist with a sufficient number of specimens to make a definitive diagnosis
is a key quality metric. It is rarely, if ever, appropriate to take fewer than
three specimens; taking this number does not increase the number of passes of
the forceps (time) needed or the expense of the procedure. Endoscopists should
also be adept at directing the biopsy forceps. Receiving an endoscopic report
with photo documentation of an abnormality but with a pathology report that is
read as normal should raise concern. The specimen should be taken with an
optimal orientation. Taking biopsies tangentially to the orientation of the
mucosa makes it difficult to provide a definitive and accurate diagnosis.
Orientation is particularly important in the duodenum, where the biopsy should
be obtained across a fold (plicae circulares) and perpendicular to the mucosa
to accurately assess villous height and crypt depth, as is critical in
assessing the diagnosis and severity of small intestinal mucosal diseases such as
celiac disease.
Most exfoliated cytologic specimens
are obtained by endoscopically guided brush cytologic procedures or
interventional radiology experts. Abrasive brush devices for obtaining tissue
for cytologic diagnoses, including an intraesophageal brush, have been proposed
as a less invasive means of diagnosing esophageal disorders. Although the risk
is lesser than with endoscopy, the procedure rarely provides definitive data
for treatment and management. Potential limitations of guided fineneedle aspirations,
whether obtained by EUS or radiology, include the risk of discomfort or
bleeding; even multiple passages of the needle may not provide adequate
cellular data. The risk of inadequate cellular data can be reduced by having a
cytology expert in the procedure room to assess the quality of such specimens.
The problem of being able to provide
definitive histologic or cytologic information for guiding treatment occurs all
too commonly with the myriad of functional gastrointestinal disorders for which
no histologic or cytologic specimen can provide a definitive diagnosis. These
disorders are particularly challenging because they are common, lead to
substantial degradation in the quality of life, and lead to a loss of
productivity and success at school or work, but they almost never lead to
serious complications or shortening of the life span. The astute clinician must
use judgment based on the risk of finding an alternative diagnosis,
particularly a life-threatening disease, to determine whether the taking of
endoscopic photographs or histologic or cytologic specimens is warranted. To
aid in this decision, various alarm signs and symptoms have been identified for
most symptom complexes. These include symptoms that persist after effective
therapy or that interrupt sleep; age over 45 years; the presence of fever,
weight loss, nausea and vomiting, or anemia; or gross blood loss. Experts have
also identified a number of criteria by which a diagnosis of a functional
disorder can be made without ordering unnecessary testing, most notably the
ROME criteria. Although they are not without controversy, such approaches provide
a means by which excessive endoscopic and radiologic testing can be minimized.