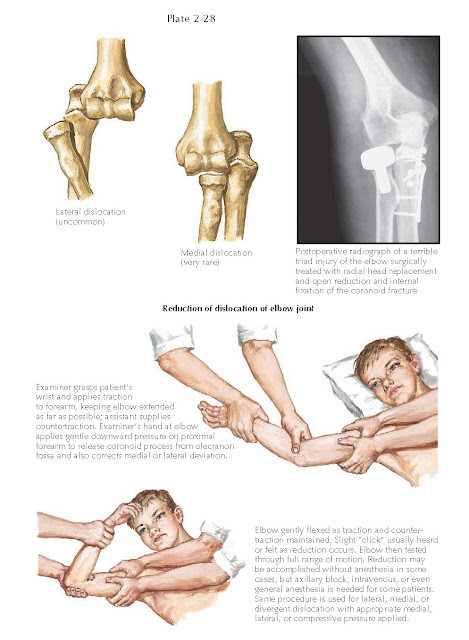
DISLOCATION OF ELBOW JOINT
Dislocations of the elbow joint are the most common dislocations after
those of the shoulder and finger joints. Swelling, pain, and pseudoparalysis of
the arm are acute signs and symptoms of dislocation, and elbow deformity is
visible on both clinical and radiographic examinations.
Acute elbow dislocations are
classified as anterior or posterior, with the direction determined by the position
of the radius and ulna relative to the humerus. In addition to the anterior or
posterior direction of dislocation, the forearm bones can also be displaced
medially or laterally. Posterior elbow dislocations are by far the most common
type and usually result from a fall on an outstretched hand. The rare, but
extensively studied, anterior dislocation of the elbow is usually an open injury
and may lacerate the brachial artery. Rarely, the radius and ulna dislocate in
different directions, an injury called a “divergent” dislocation.
Dislocations of the elbow result in a
pattern of ligamentous injury that depends on the direction of dislocation. For
posterior dislocations, the ligamentous injury typically starts laterally,
disrupting the lateral collateral ligament complex first; it then moves medially,
disrupting the anterior and posterior joint capsule, followed by the medial
collateral ligament complex. Elbow dislocations are sometimes accompanied by
fractures as well, including fractures of the medial or lateral epicondyle,
olecranon, radial head or neck, or coronoid process of the ulna. As discussed
previously, the combined injury pattern of an elbow dislocation associated with
both a radial head fracture and a coronoid fracture has been termed a terrible
triad injury.
Fracture-dislocations of the elbow,
especially displaced fractures of the olecranon, coronoid process, and radial
head, often require surgical fixation to ensure longterm stability and function
of the joint. An avulsed medial epicondyle can become wedged inside the joint
during reduction of the dislocation. Only occasionally can closed manipulation
free the avulsed fragment from within the joint; arthrotomy is usually needed
to remove the fragment and return it to its anatomic position.
Reduction Of Dislocation Of Elbow
Joint
A posterior dislocation of the elbow
is reduced with distal traction. While an assistant secures the proximal
humerus, the examiner applies traction in the line of the forearm, holding the
forearm supinated, and then gently flexes the elbow joint to allow the humerus
to reduce into the olecranon fossa. If the elbow is reduced immediately after
dislocation, complete muscle relaxation may not be needed; if treatment is
delayed, conscious sedation, axillary block, or general anesthesia is used to
induce complete muscle relaxation. Radiographs should be obtained after
reduction to confirm that the elbow joint is concentrically aligned. The neurovascular
status of the distal limb is checked both before and after reduction. Any
changes or abnormalities suggest entrapment of a nerve or vessel during
reduction, which must be relieved promptly to prevent a long-term deficit.
After the initial reduction, the
examiner moves the elbow through a full range of motion to assess its stability
and to check for crepitus in the joint. Crepitus strongly suggests loose
fracture fragments in the joint. If the elbow remains stable through a full
range of motion, it is immobilized in 90 degrees of flexion in a posterior
splint. The neurovascular status of the limb is monitored frequently while the
elbow is splinted to ensure that a deficit does not develop. Most isolated
elbow dislocations are treated with splint immobilization for a short period of
time (1 to 2 weeks) before beginning range-of-motion exercises. The exercises
should be gentle initially but as active as symptoms permit. The physician’s
assessment of the degree of stability after reduction helps determine what
range of motion to allow and when to begin the exercise program.
Elbow dislocations cause few long-term
complications. By far the most common is residual joint stiffness, particularly
loss of extension. Although some degree of stiffness almost always persists,
early active motion can minimize this problem. The older the patient, the
earlier active elbow movement should be started.
Myositis ossificans, another
complication of elbow dislocation, results from muscle injury at the time of dislocation.
Myositis ossificans is more likely to develop after severe injuries, such as
those that are high energy or associated with fractures, and when treatment has
been delayed. Early passive motion is discouraged in patients with dislocation
and muscle injury because excessive muscle stretching may precipitate the development
of myositis.
Recurrent dislocations after an
isolated elbow dislocation are uncommon and are thought to be due to extensive
collateral ligament damage (medial and lateral) or an occult fracture. Surgery
to repair or reconstruct the collateral ligaments may be necessary in this situation.