Odontogenic Infections: Their Spread and Abscess
Formation
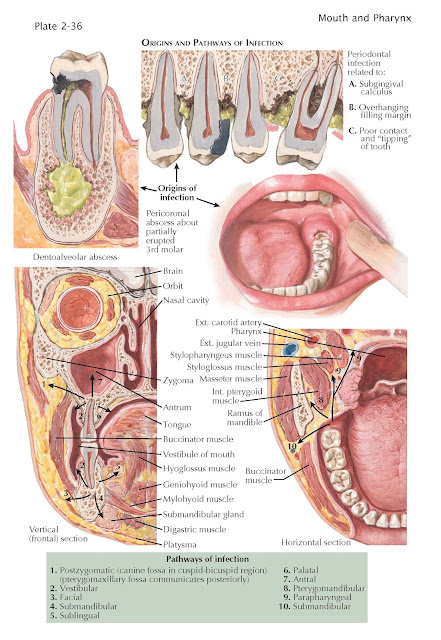
The most frequent causes of inflammatory swellings
of the jaws, the middle and lower thirds of the face, and the upper part of the
neck are infections of the teeth, with the pulp canal or the periodontal
membrane as the primary focus. The dentoalveolar abscess is the most
frequently encountered dental infection. It is usually the end result of dental
caries; more rarely, it originates in a tooth devitalized by trauma. The
abscess may develop very acutely and burrow through bone to lodge under the
periosteum, which it then perforates to induce an intraoral or a facial
abscess. In other instances, a more chronic inflammatory process leads to an
organized granuloma at the root apex, which may remain dormant for years,
evolve slowly into a sterile cyst, or develop into an acute alveolar abscess.
While the abscess is confined to the bone, pain and extreme tenderness of the
involved tooth are the characteristic symptoms. By the pressure of edema, the
tooth is extruded from its socket, so that each contact with the teeth of the
opposing jaw aggravates the pain.
The periodontal abscess is the
second most common odontogenic infection. It arises from an ulcerated
periodontal crevice (pocket), which is created by the loss of attachment (poor
contact) between the tooth on one side and the investing gingiva,
periodontal membrane, and bone on the other. This periodontitis occurs with
increasing severity in older age groups and is the most prominent etiologic
factor in the loss of teeth. Calculous deposits, traumatic occlusion, irritating
filling margins, implanted teeth, and other factors may play a contribut-
ing role. A third odontogenic infection, the pericoronal abscess, originates
in a traumatized or otherwise inflamed flap of gingiva overlying a partly
erupted tooth, usually a lower third molar.
Odontogenic infections involve the
soft tissues chiefly by direct continuity (the numbered pathways are
illustrated in the drawings). Lymphatic spread plays a secondary role, and
hematogenous dissemination rarely results in a facial abscess. Bacteremia, however,
is common and has been demonstrated as a transient phenomenon arising from
chewing or manipulation of apically or periodontally infected teeth. Local
extension follows the line of minimal resistance chosen based on the tooth and
its anatomic proximity to the bone, fascia, and muscle attachment. Where the
muscle layers act as a barrier, extensive cellulitis may spread along the
fascial planes of the head and neck. Infections from the maxillary teeth may
perforate the cortical bone of the palate, the vestibule, or the regions
separated from the mouth by attachments of the muscles of facial expression or
the buccinator muscle. Those from the incisor teeth tend to involve the upper
lip; from the cuspids and premolars, the canine fossa; and from the molar teeth,
the infratemporal space or mucobuccal fold. The vestibular abscess is
generally localized and is not accompanied by excessive edema, owing to the
softness of the tissues and lack of tension. In the advanced stage, a shiny
fluctuant swelling is visible at the region of the root apex or somewhat below
it. Abscess (postzygomatic) of the canine fossa usually bulges into the
buccal sulcus but is chiefly marked by swelling of the infraorbital region of
the face and the lower eyelid. The upper lid, the side of the nose, and the
nasolabial fold and upper lip may be involved by edema.
Infections of the mandibular teeth may
give rise to swellings of the vestibule or the sublingual, submental, or
submandibular space. Abscess of the submandibular region is encountered
with infections of the premolar and molar teeth. The classic sign is a large
visible swell- ing below the mandible, extending to the face and distorting the
lower mandibular border; it is extremely tender and accompanied by trismus. A
submandibular space abscess may easily pass into the sublingual space (5) along
the portion of the gland that perforates the mylohyoid muscle. This results in
elevation of the floor of the mouth and displacement of the tongue to one side.
The submental area may be invaded by passage of pus past the digastric muscle,
resulting in a general swelling of the entire submandibular region. A
dentoalveolar abscess from a lower molar tooth is capable of producing the most
serious and fulminating infections of the submandibular (4), pterygomandibular
(8), and parapharyngeal (9) pathways. A pterygomandibular abscess results in
deep-seated pain and extreme trismus, with some deviation of the jaw owing to
pterygoid muscle infiltration. Infection in this space may, in exceptional
cases, enter the pterygoid and pharyngeal plexuses of veins and result in a
cavernous sinus thrombosis. A parapharyngeal abscess causes bulging of the
pharynx, with equally marked trismus.
The onset of facial cellulitis is
heralded by edema of the soft parts, often quite extensive and without
discernible fluctuation. Pain increases with pressure and induration. As
abscess formation progresses, the central area reveals pitting edema and
eventually becomes shiny, red, and superficially fluctuant. Pain and tenderness
are related to pressure and induration. A fever of 38.5° to 40° C,
leukocytosis, and severe toxemia are characteristic. Trismus occurs when the
elevator muscles are affected by inflammation or reflex spasm caused by pain.
In some cases, rather than the typical production of an abscess, a chronic
cellulitis follows the acute phase, with persistent, deeply attached swelling.
A phlegmon may be apparent from the onset, with a brawny, indurated distention
of muscular and subcutaneous layers, devoid of exudate and showing no
tendency to localize.
Ludwig angina, a purulent inflammation, begins as a phlegmon in
the submandibular space, usually after a molar tooth infection or extraction,
and rapidly spreads to occupy the submandibular region, bounded inferiorly by
the hyoid bone. The floor of the mouth and tongue are raised through
infiltration of extrinsic and intrinsic muscles. The hard, dusky swelling
descends to the larynx, where edema of the glottis, combined with the pressure
of the tongue against the pharynx, interferes with respiration. In addition to
the usual flora of odontogenic infections (alpha, beta, and gamma strep-
tococci and, occasionally, gram-negative bacilli), the bacterial picture in
true phlegmon tends toward anaer- obic organisms, or facultative anaerobes, and
gangreneproducing mixed groups such as the fusospirochetal combination.
Osteomyelitis may produce cellulitis or abscess similar to the
odontogenic variety. Its chief incidence is as a complication following a
traumatic extraction, particularly if performed in the presence of acute
infection, or a comminuted fracture involving the roots of teeth. Occasionally,
it is the result of an abscess contiguous to a large area of bone, and it
typically begins in the lower third molar region. Sclerotic or dense bone is
more easily deprived of nutrition through trauma and at increased risk for
developing an abscess following tooth extraction. Symptoms include those of
cellulitis, with intermittent, deep, boring pain, and sequestrum and involucrum
formation, seen on radiographic imaging in late stages. Symptom and
radiographic resolution results from therapeutic intervention with abscess
drainage and antibiotic therapy.
A fracture of the mandible or
maxilla is always compound where teeth are present, causing the line of
fracture to be contaminated by normal oral flora that seldom produces
infection; however, with projection of a tooth root in the line of fracture,
suppuration typically develops. An externally compounded fracture is more prone
to develop sepsis than a noncomminuted or simple nondisplaced fracture.
Actinomycosis is a specific infection that occurs centrally in
the jaws or peripherally in the soft tissues, where it forms an indurated
swelling with multiple fistulae of the skin, resembling a chronic odontogenic
abscess. Because this is an obligatory oral pathogen, inoculation is usually
through damaged mucosa, most often following oral surgery or recent dental work
and less often following trauma or local radiation therapy. The diagnosis is chiefly
made by a smear of the exudate, which contains peculiar granular yellow bodies (sulfur
granules) and the specific organism (Actinomyces bovis) that causes
the disease. Culture of the organism is unreliable, and biopsy may be required
to establish the diagnosis.