Elbow fractures are more
common in children than adults, and treatment can differ greatly from adults
because of the healing and remodeling potential of pediatric fractures. Occult
fractures are also more common in children, in part because not all of the
damaged bone may be ossified. Detecting unossified fractures on plain
radiographs can be difficult, and many of the epiphyses in the elbow region
ossify late. Comparison radiographs of the uninjured elbow often help in
identifying subtle fracture lines and displaced fracture fragments. Any child
who presents with a history of fall or injury, tenderness to palpation about
the elbow, and a fat pad sign on plain radiographs should be treated for an
occult fracture and immobilized in a splint or cast for a minimum of 3 weeks.
New callus formation at the presumed fracture site will typically be present on
plain radiographs at this time to allow the diagnosis to be confirmed.
Supracondylar Fracture Of
Humerus
Supracondylar fractures of the
humerus are the most common elbow fracture in children and are much more common
in children and adolescents than in adults. In children, the fracture typically
involves the thin bone between the coronoid fossa and the olecranon fossa of
the distal humerus, proximal to the epicondyles, and the fracture line angles
from an anterior distal point to a posterior proximal site. In adults,
supracondylar fractures are not usually confined to the extra-articular portion
of the distal humerus, as in children, but extend into the elbow joint.
The most frequent cause of
supracondylar fractures of the humerus is a fall on the outstretched hand with
the elbow extended. By far the most common fracture pattern is an
extension-type injury with posterior displacement of the distal fragment; only
5% to 10% of supracondylar fractures are flexion-type injuries with anterior
displacement of the distal fragment. Extension-type supracondylar fractures are
classified as nondisplaced (type I), partially displaced with the posterior
cortex still intact (type II), and completely displaced with no cortical
contact between the fragments (type III).
In the evaluation of any
fracture, careful assessment of the neurovascular status is important, but this
assessment is even more critical in supracondylar fractures of the elbow
because of the proximity of the brachial artery and median nerve to the distal
spike of the proximal fragment. Neurologic injury or vascular insult and
Volkmann ischemic contracture can result from this type of fracture. A direct
neurovascular injury may occur from the fracture spike, or neurovascular compromise
may occur from severe swelling that accompanies the injury.
Before reduction, the
fractured elbow should be splinted in extension so that arterial circulation is
not compromised by flexion of the distal fragment. When the injury is evaluated
in the emergency department, the neurovascular status of the limb should be
carefully determined and monitored. The first focus of management is on
reduction of the displaced fracture fragments to alleviate any neurovascular
compression if it is present. The supracondylar fracture should be reduced as
soon as possible after injury, preferably with the patient under conscious
sedation or general anesthesia. Closed reduction is carried out by gentle
distraction in the line of the forearm until the humerus is restored to its
full length. The medial or lateral angulation is corrected, and in
extension-type injuries the elbow is flexed greater than 90 degrees for added
stability. With the elbow in extreme flexion, the posterior periosteum and the
aponeurosis of the triceps brachii muscle act as a hinge to maintain the
reduction of the fragments. In more stable fractures (some type II fractures),
this posi- tion may be secure enough with a plaster splint or long-arm cast
alone for 4 to 6 weeks to prevent redisplacement of the fracture fragments and
allow healing.
In assessing the reduction
achieved, displacement in the anteroposterior plane is not nearly as important
as the presence of lateral or medial angulation. If the fracture heals with the
distal fragment tilted medially or laterally, a significant deformity, either
cubitus varus or cubitus valgus, results. Varus or valgus angulation after
reduction is best diagnosed on an anteroposterior
radiograph or a Jones view of the elbow, which reveals a lack of contact
between the two bone fragments on one cortex.
If the adequacy of the
reduction or if the vascular supply of the limb is in question, the fracture
should be treated either with percutaneous pin fixation performed under image
intensification or with open reduction and internal fixation. Type III
fractures and many type II fractures require pin fixation for stability. Image
intensification allows closed reduction of the fracture and percutaneous
insertion of two or three Kirschner wires. Open reduction is usually done
through a lateral approach to the distal humerus. Pins can be passed in a
crossed (medial and lateral pins) or divergent (all lateral pins) pattern, with
care to avoid injury to the ulnar nerve when placing any medial pins. After
internal fixation, the elbow can be splinted in any angle of flexion to avoid
compromising the function of the brachial artery. Vascular exploration and/or
repair is rarely needed but may be indicated if a pulseless, unperfused
extremity does not improve after fracture reduction and operative fixation.
The major long-term
complication of very severe fractures is a change in the carrying angle of the
elbow, primarily cubitus varus, owing to incomplete or loss of reduction at the
time of treatment. The normal carrying angle of the elbow (10 to 20 degrees of
valgus) is decreased or reversed. Despite the abnormal appearance of the elbow,
function is not typically compromised, even with a severe varus deformity.
Closed or open reduction and percutaneous pinning of unstable fractures (types
II and III) are used to prevent varus deformity. Angular malunions that result
in a significant loss of function or cosmetic deformity are best treated with a
corrective osteotomy at the site of the original fracture. The alignment of the
corrective osteotomy is maintained with a plate and screws or an intramedullary
nail. The osteotomy is often supplemented with cancellous bone grafts to ensure
healing. Neurologic injury, although not common, does occur and can involve
either the median, radial, or ulnar nerve, with median nerve injury the most
common. Vascular injury is a devastating complication because it can lead to
Volkmann contracture from a resulting missed compartment syndrome. Regardless
of the reduction and fixation method, care should be taken once the limb is
splinted or placed in a cast to closely monitor it for adequate circulation and
a stable neurologic examination. Distal pulses may not always be easily
palpable owing to vascular spasm from the injury, but if distal perfusion and
capillary refill are normal with no evidence of compartment syndrome then the
limb is likely stable. Finally, all elbow fractures can potentially result in
decreased motion and stiffness.
 |
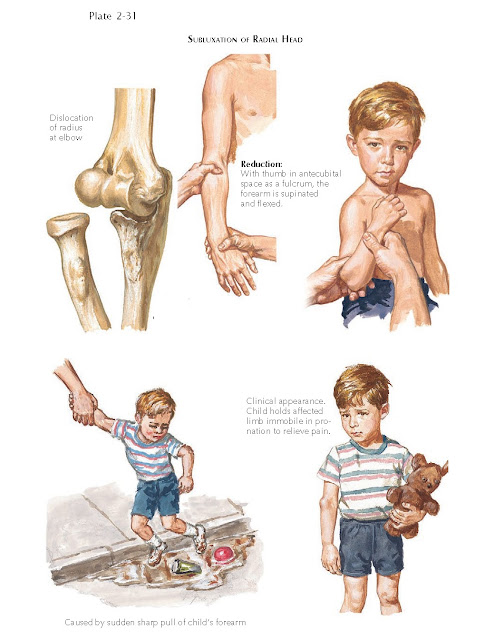
| SUBLUXATION OF RADIAL HEAD |
Fractures Of Lateral
Condyle
A lateral condyle fracture is
the second most common elbow injury in children. Typically, it occurs as an
avulsion injury of the attached extensor muscles. If not reduced well and
securely fixed, this type of fracture tends to lead to significant long-term
problems, includ- ing nonunion, cubitus valgus, and tardy ulnar neuropathy.
Growth arrest of the lateral humerus produces a progressive valgus deformity of
the joint, which, in turn, may lead to ulnar nerve palsy later in life.
Non-displaced fractures of the lateral condyle can be treated with
immobilization in a cast. However, because of a significant risk of late
displacement of the fracture, the patient must be monitored with frequent
radiographic examinations during the first 2 weeks after injury. Displaced
fractures require open reduction and pin or screw fixation to maintain a
satisfactory reduction and avoid the deformity and neurologic complications
asso- ciated with this injury.
Fractures Of Medial
Epicondyle
This injury is the third most
common elbow fracture in children. It results from a valgus stress applied to
the elbow causing an avulsion injury of the medial epicondyle due to
contraction of the flexor-pronator muscles. The fracture is frequently
associated with a posterior or lateral dislocation of the elbow joint.
Dislocation causes the strong ulnar collateral ligament to pull the
epicondyle fragment free from the humerus. During reduction of the dislocation,
the fragment sometimes becomes trapped in the elbow joint. If not incarcerated
in the joint, the fragment may be slightly displaced or rotated more than 1 cm
away from the distal humerus. A significantly displaced fragment is sometimes
easily palpable and freely movable on the medial aspect of the elbow joint.
Nondisplaced and minimally
displaced fractures heal well with splint or cast immobilization. A displaced
fragment trapped in the joint as a result of an elbow dislocation requires open
reduction to restore joint congruity and stability. Significantly displaced
fragments outside the joint may not heal, and some surgeons recommend open
reduction and internal fixation. However, even if the fragment fails to unite,
long-term complications are few.
Fracture Of Radial Head Or
Neck
During a fall on the
outstretched hand, the radial head or neck may fracture as it impacts against
the capitellum, typically from a valgus stress on an extended elbow. Fractures
are usually through the proximal physis and into the radial neck in a Salter II
pattern. Significant angulation of the radial head fragment may occur, and if
the angulation is greater than 30 degrees the fracture should be reduced with
closed manipulation. Reduction is achieved using digital pressure over the
angulated head while alternatively supinating and pronating the forearm.
Although closed reduction is sufficient for most fractures, severely displaced
or angulated fractures of the radial head require percutaneous or open
reduction and internal fixation. Even completely displaced fragments should be
reduced and fixed in place. In a growing child, the radial head should never be
excised, because excision always leads to sig- nificant loss of elbow function.
Dislocation Of Elbow Joint
This childhood injury is less
frequent in younger children but commonly seen in boys between 13 and 15 years
of age and is frequently associated with athletic injuries. Apparent elbow
dislocations in young children or infants should raise concern for a
transphyseal fracture of the distal humerus that is the result of child abuse.
Radiographs of these fractures may be confused for dislocations because of the
lack of ossification of the distal humerus at this age. Most elbow dislocations
in children are posterior, as in adults. Associated avulsion fractures of the
elbow, particularly avulsion fractures of the medial epicondyle, can occur.
With adequate anesthesia, most elbow dislocations can be reduced easily. The
elbow is initially placed in a splint after reduction; and for stable, isolated
injuries, the management is similar to that for adults.
Subluxation Of Radial Head
This injury, also known as
nursemaid elbow, is the most common elbow injury in children younger than 5
years of age and results from longitudinal traction applied to the limb. The
annular ligament moves proximally and becomes interposed between the radius and
ulna, causing the radial head to subluxate. Clinical findings are
characteristic: the injured limb hangs dependent and the child avoids arm use,
the forearm is pronated, and any attempt to flex the elbow or supinate the
forearm produces significant pain. Radiographs do not show any significant bone
abnormality about the elbow. Physical examination almost always reveals
localized tenderness over the radial head. In most patients, reduction can be
achieved by complete supination of the forearm, pressure on the radial head,
and subsequent elbow flexion. Although this causes a moment of fairly severe
pain, supination causes the radial head to slide back into its normal position,
and frequently a “click” is felt as the annular ligament slides back around the
radial neck. Reduction brings almost immediate and complete relief of pain; and
within a few moments, the child begins to use the elbow. If the closed
reduction is successful, immobilization is not necessary. The physician should
explain the cause of the subluxation to the child’s parents and tell them to
avoid longitudinal traction on the limb. The risk of recurrent subluxation is
minimal.