Oral
Manifestations in Various Skin Conditions
A great number of pathologic conditions of the
skin have accompanying oral manifestations that may precede or occur
concurrently with or independent of the cutaneous eruption. In general, such
lesions do not bear strict comparison with the skin lesions, because of the
considerable difference in moisture, temperature, exposure to trauma, lack of a
keratin layer, and the presence of secondary infection. In the differential
diagnosis the prevalence of purely local lesions of a vesicular or bullous type
(e.g., recurrent aphthous ulcers) should be kept in mind.
One of the familiar dermatoses
in which the oral mucosa may participate is lichen planus, which is a
chronic inflammatory disorder with no malignant potential. It has the
appearance most commonly of rectangular white plaques associated with erythema
and erosions; less often seen are ulcerations and hyperkeratotic plaques. The
pathogenesis has not been completely elucidated, but it involves a T
cell–mediated immune response causing a cytotoxic reaction by activating CD8 T
cells against epithelial basal cells. The diagnosis is confirmed through a
review of the patient history, physical examination, and histologic findings.
The presence of the purplish, polygonal, or angular skin papule eruptions
improves the accuracy of the diagnosis. In a majority of cases, however, the
oral lesions precede those of the skin surfaces, and, not infrequently, the
disease may remain confined to the mouth. Most often, the cheek mucosa displays
the characteristic fine, lacelike pattern of bluish white lines and small,
pinhead-size, elevated papules, although the tongue, palate, and gingiva may be
similarly affected. The latter locations, as compared with the cheek, usually
show coarser plaques and aggregated papules. The lips are least commonly
involved. Occasionally, an erosive form may be observed, which is painful and
characterized by a caked, whitish material covering a red base in which
bleeding is easily induced. The radiating and interlaced grayish white lines
are the most significant signs in the diagnosis. These lesions are most often
seen in HIV/AIDS and other immunosuppressed conditions. Differentiation from
syphilis, moniliasis, and glossitis migrans is easily made, but differentiation
from other local leukokeratoses is sometimes difficult, and biopsy then becomes
a helpful adjunct. The histopathologic picture in lichen planus shows moderate
keratosis or parakeratosis, a “sawtooth” arrangement of the rete pegs, and a
very typical band of lymphocytes chiefly concentrated beneath a vague basal
cell zone. This lymphocytic infiltrate is sharply demarcated from the rest of
the stroma.
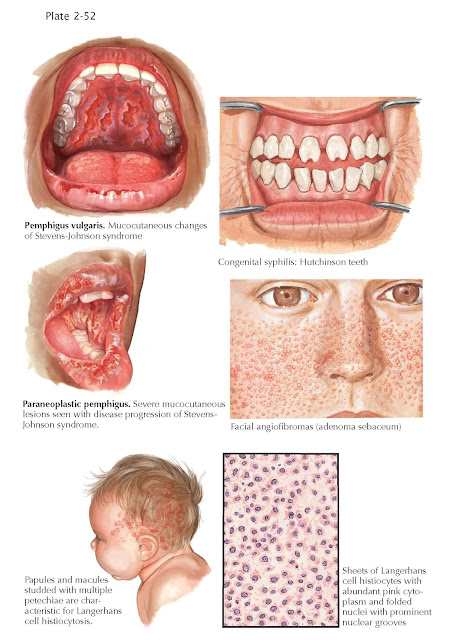
Pemphigus begins in over 50% of cases with
manifestations on the oral mucosa, where large, painless vesicles or bullae
develop. The thin-walled blebs rupture in a short time, leaving a superficial ulcer
rimmed with tattered, grayish shreds of thin membrane. Signs of inflammatory
reactions are absent in the early stages but may present themselves later in
the form of a slightly red halo. The onset is insidious, chronicity and
recurrence being typical even when unaccompanied by skin signs. As the disease
progresses, confluent areas become raw and oozing, and salivation, pain, and
bleeding increase; mastication and swallowing are impaired. Erythema
multiforme major may affect, along with the skin, the mucous membranes of
the mouth, eyes, and anogenital regions. Erythema multiforme minor presents
similarly but without any mucosal involvement. Both the major and minor forms
have the distinctive target skin lesions. The earliest vesicular lesions in the
mouth are sometimes indistinguishable from those of pemphigus. A diffuse
bullous stomatitis ensues, with a heavy yellowish pseudomembrane, a marked
variation in the size of the lesions, and, often, a bluish red areola around
the lesions. The lips are usually swollen, ulcerated, and covered with
hemorrhagic crusts. The severity of the disease varies. Recurrence is common
and tends to be seasonal. Although the development of erythema multiforme has
been linked to many factors, including but not limited to, medications,
malignancy, autoimmune disease, and herpes simplex virus infection, the virus
is the precipitating agent in over 90% of cases.
Stevens-Johnson syndrome is a rare acute, life-threatening
mucocutaneous disease that is nearly always triggered by a drug. Most often the
offending agents are allopurinol, anticonvulsants, antimicrobial agents, and
nonsteroidal medications. The cutaneous reaction includes extensive
keratinocyte cell death causing separation of areas of skin at the
dermal-epidermal junction. The oral mucosa and the vermillion border are almost
invariably involved with painful hemorrhagic erosions covered with a grayish
white membrane. Stomatitis and mucositis lead to impaired oral intake, with
consequent malnutrition and dehydration. The degree of body surface area
involved in the skin separation process in Stevens-Johnson syndrome is up to
10%. Toxic epidermal necrosis is a further progression of the cutaneous
process, resulting in involvement of more than 30% of the body surface area. If
the involvement is between 10% and 30%, the disease is classified as a
combination of Stevens- Johnson syndrome and toxic epidermal necrosis.
Acquired epidermolysis
bullosa is an autoimmune
subepithelial blistering disease that primarily affects elderly individuals; it
has no predilection for gender or race. The skin eruption is generalized and
favors skin folds and flexural areas. The initial presentation is an area of
localized erythema or urticarial papules that coalesce into plaques and
subsequently turn into dark-red vesicles and bullae in a few weeks. Oral
blisters can develop; they are few in number and are less severe and more
transient than the cutaneous lesions. Hereditary epidermolysis bullosa is
a heterogeneous group of genetic bullous disorders characterized by blister
formation in response to mechanical trauma. The dystrophic and junctional types
are more serious and include organ involvement, skin breakdown, and scarring.
Enamel hypoplasia is present in, and limited to, the junctional form, causing
pitting of the deciduous and permanent surfaces of the teeth. Dental caries is
prominent in both the junctional and dystrophic forms of the disease. None of
the serious cutaneous or oral manifestations have been described in the simplex
form of the condition.
Langerhans cell
histiocytosis (histiocytosis X) is a rare disorder characterized by organ infiltration of Langerhans cells.
Papules, vesicles, nodules, and a seborrheic-like pattern on the scalp and
diaper area are the primary cutaneous findings of the disease. Dental problems
are seen in 30% of patients, and they include a destructive periodontitis
resulting from osseous infiltration of the Langerhans cells. Ultimately this
can cause destruction of the dentition support system from the maxilla and
mandible and loosening of the teeth (floating teeth). Periodontal
involvement characterized by gingival recession and pocket formation ultimately
leads to alveolar bone loss, culminating in loss of dentition.
Congenital erythropoietic
porphyria is a rare autosomal
recessive disorder that is phenotypically depicted as an abnormality of heme
biosynthesis. A pale oral mucosa and teeth that appear a red-maroon color (erythrodontia)
are the primary dental abnormalities seen. The pattern of discoloration is
distinct and aids in the diagnosis. The incisors are nearly completely stained,
whereas the canines are colored at the cusp tips and the molars demonstrate
varying degrees of discoloration. The coloring of the teeth is thought to be
from an affinity of porphyrins for the calcium phosphate rich teeth.
Congenital syphilis is a result of transplacental infection by
Treponema pallidum. Cutaneous findings of red macules and papules, a
papulosquamous eruption, or a desquamating dermatitis are seen in less than
half of the infants infected, but hemorrhagic bullae on the palms and soles are
pathognomonic of the infection. Rhinitis, mucous patches on the lips, mouth,
tongue, and palate, and condylomata mainly in the anogenital area and angles of
the mouth are characteristic.
Ectodermal dysplasias constitute a group of hereditary
conditions characterized by one or more ectodermal structures, including the
skin. The typical areas affected are the hair (hypotrichosis, partial or
complete alopecia), nails (dystrophic, hypertrophic, or abnormally keratinized),
tooth enamel (defects or absent), and hypoplastic or aplastic sweat glands.
Dental defects are characteristic and a core manifestation of the disease,
including anodontia, polyodontia, dysplastic teeth, retained primary teeth,
deficient enamel development (amelogenesis imperfecta), and underdevelopment of
the alveolar ridge.
Tuberous sclerosis
(Bourneville disease) has
an autosomal dominant inheritance. It
results in the
formation of hamartomatous
lesions in several organ systems, including the skin, brain, kidney, ear, lung,
bone, and eye. Characteristic oral lesions include gingival fibromas and dental
enamel pits caused by a reduced amount of enamel present during dentition
development. The pits are large defects in the enamel without a change in color
or texture of the enamel surrounding the pit, producing a pockmarked
appearance.
Nevoid basal cell carcinoma
syndrome is an autosomal
dominant predisposition for the development of epitheliomas, medulloblastomas,
and other developmental abnormalities. The hallmark of the disease, however, is
the presence of multiple odontogenic keratocysts. Finding the keratocysts in a
young child is diagnostic of the condition.