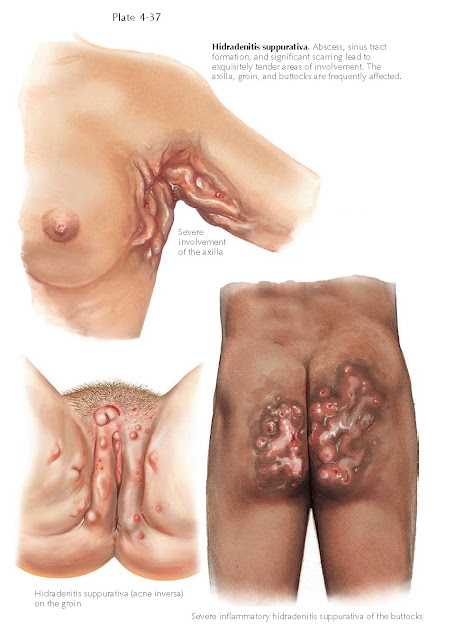
HIDRADENITIS
SUPPURATIVA (ACNE INVERSA)
Hidradenitis suppurativa (acne inversa) is a
rare chronic, life-altering disease. It can be an isolated clinical finding, or
it can be associated with cystic acne, dissecting cellulitis of the scalp, and
pilonidal cysts.
Clinical Findings: Hidradenitis suppurativa is most commonly
encountered in postpubertal women. The ratio of female-to-male involvement is
approximately 4:1. This condition preferentially affects areas that are rich in
apocrine glands and terminal hairs. The areas most commonly involved are the
axillae, groin, and inframammary folds. It is rare in other areas. Hidradenitis
suppurativa starts as tiny red papules or nodules that tend to be
folliculocentric. The papules are tender and firm to palpation. At this point,
the differential diagnosis includes an early folliculitis or furunculosis. As
the disease progresses, the hard nodules become fluctuant and spontaneously
drain to the surface of the skin. The nodules may coalesce into plaques with
varying amounts of scarring. The longer the process has been going on, the more
scarring is prevalent. Eventually, sinus tracts develop that interconnect multiple
subcutaneous nodules with multiple cutaneous openings.
Clinically, pressing on one of the nodules may produce drainage from a distant
sinus tract. The disease is relentless, and new crops of lesions repeatedly
develop. Pain is significant and is a main cause of morbidity. Obesity tends to
be seen in association with hidradenitis suppurativa. Hidradenitis has been
seen in association with Crohn’s disease, and some believe that hidradenitis
suppurativa is a cutaneous form of Crohn’s disease. Long-standing disease has
been associated with the development of squamous cell carcinoma. The tumors
tend to be large at diagnosis
The drainage from the cutaneous
nodules often requires extensive bandaging to keep clothing from getting
soiled. The drainage has a malodorous, foul smell. The draining sinus tracts
and nodules are often colonized with various bacteria, and cultures of the
purulent drainage show growth of a number of different organisms, including Staphylococcus
aureus and streptococcal species. However, this is not primarily an
infectious disease. The bacteria in these cases are present secondary to the
underlying inflammatory condition and the lack of normal cutaneous skin barrier
function. Pathogenesis: Hidradenitis suppurativa is an
inflammatory disease with secondary bacterial superinfection and colonization.
Routine culturing of the nodules and the drainage is often sterile.
Hidradenitis is theorized to be caused by rupture of the mature follicular
epithelium along areas of apocrine glands; hence, its propensity to occur in
areas with high densities of apocrine glands. A hormonal control over the
process has been theorized, given that it is more common in postpubertal women
and in obese individuals. Once the hair follicle ruptures, an inflammatory
cascade is set off and causes the resulting nodules, cysts, fistulas, and
scarring. It appears to be a self-perpetuating process. The exact mechanism
by which this occurs is unknown.
Histology: Chronic lesions show a dense, mixed
inflammatory infiltrate with abscess and sinus tract formation. Varying amounts
of fibrosis and scar tissue are present. Apocrine gland inflammation can be
appreciated in a fair number of cases. The inflammation extends into the
subcutaneous tissue.
Treatment: Therapy is often aimed at reducing inflammation
and bacterial superinfection. There is no curative therapy, and most treatments
have only anecdotal reports of success. Topical
clindamycin and other antibacterial products such as benzyl peroxide are often
the first-line agents employed for mild disease. Oral antibiotics, typically in
the tetracycline class, are often used because they have both antiinflammatory
and antibacterial properties. Weight loss must be advocated. Other agents that
have had limited success include isotretinoin, etanercept, and infliximab.
Surgical options include wide local excisions to remove the affected
tissue and repair with complex flap closure. Liposuction has also been tried in
an attempt to remove the affected apocrine gland hair follicle unit. The only
potential for cure is with a surgical approach. This approach seems to work
best for axillary disease; groin and inframammary disease almost always recurs
after surgery. It is also of the utmost importance to address patients’
psychosocial needs, because this disease has a devastating toll on the
patients it afflicts.