VOCAL CORD DYSFUNCTION
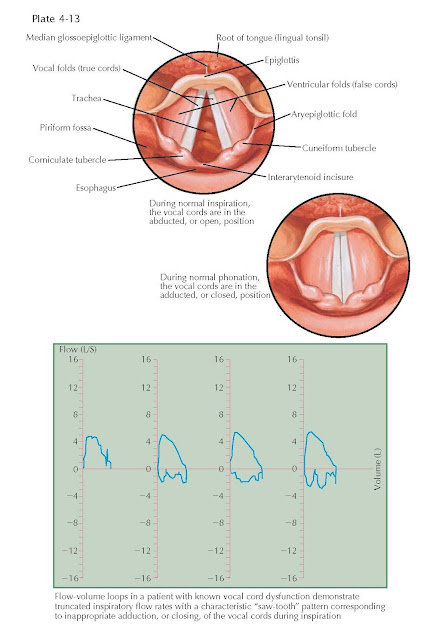
Vocal cord dysfunction (VCD), also known as
paradoxical vocal cord motion (PVCM), is a relatively poorly understood
laryngeal disorder manifest by inappropriate adduction, or closing, of the
vocal cords during inspiration. This is in contrast to the normal respiratory
cycle, in which the vocal cords are abducted, or open, during inspiration and
only begin to adduct toward the end of exhalation or with the onset of phonation.
Physiologically, partial adduction of the vocal cords at the end of the
expiratory phase maintains alveolar patency by generating positive
end-expiratory pressure. Full adduction of the vocal cords occurs normally
during phonation. As air expelled from the lungs encounters a closed glottis,
subglottic air pressure increases, which in turn provides the force necessary
to vibrate the vocal cords and produce voice. In contrast, paradoxical
adduction of the vocal cords during inspiration in patients with VCD results in
acute, intermittent episodes of functional airway obstruction.
The
most common symptoms of VCD are inspiratory stridor, dyspnea, hoarseness,
throat tightening, and cough. Unfortunately, these symptoms are relatively
nonspecific and may mimic other conditions such as asthma, epiglottitis,
angioedema, or anaphylaxis. Many patients with VCD will have been treated
aggressively for presumed asthma without improvement. In contrast to asthma,
the airway obstruction in VCD occurs with inspiration rather than expiration,
and laryngeal stridor should not be mistaken for bronchial wheezing. Pulmonary
function testing can help exclude asthma and support a diagnosis of VCD, with
attenuation of the inspiratory flow rate on flow-volume loops. It is common to
have both asthma and VCD, in which case methacholine challenge testing is often
helpful.
A
diagnosis of VCD can be further substantiated with transnasal flexible fiberoptic
laryngoscopy. As with pulmonary function testing, this should be done while the
patient is symptomatic. Because of the episodic nature of VCD, it may be
necessary to first challenge the patient with exercise, sustained vocal tasks,
or other known triggers to elicit an acute exacerbation. Flexible laryngoscopy
demonstrates a structurally normal larynx with paradoxical adduction of the
vocal cords during inspiration. This is more pronounced when breathing in
through the mouth rather than the nose, which provides a stronger neural
stimulus for vocal cord abduction. Adduction of the anterior two-thirds of the
vocal cords with a diamond-shaped posterior glottic gap is most commonly
described, although additional findings of false vocal cord adduction and
anterior to posterior supraglottic constriction have been reported.
The
cause of VCD is poorly understood. Because of the lack of clear organic
pathology and the high incidence of underlying psychiatric conditions in these
patients, VCD has historically been considered a psychogenic disorder, as
evidenced by such antiquated terms as Munchausen’s stridor and factitious
asthma. Although VCD may be a manifestation of a somatization or conversion
disorder in some patients, nonpsychogenic causes must also be considered.
Brainstem compression, upper or lower motor neuron injury, and movement
disorders have been associated with VCD. Laryngeal hyperresponsiveness
secondary to laryngopharyngeal reflux (LPR) has also been implicated as a
potential causative factor in VCD. A diagnosis of LPR is supported by findings
of posterior laryngeal erythema, interarytenoid mucosal pachydermy, and
posterior pharyngeal cobblestoning on flexible laryngoscopy. The treatment of
VCD involves a multifaceted approach, with identification and elimination of potential
irritants or triggers, medical therapy for underlying psychogenic or pathologic
conditions, and intensive behavioral therapy with an experienced
speech-language pathologist focusing on laryngeal relaxation and diaphragmatic
breathing techniques. If necessary, severe attacks may be managed acutely with
anxiolytics, heliox, or continuous positive airway pressure ventilation. Most
patients with VCD improve with proper treatment and time.