DEFORMITIES OF THE METACARPOPHALANGEAL
JOINTS
Arthritic diseases may affect any joint, but their
effect on the hands can be especially devastating. The disease process attacks
the joints, ligaments, and tendons, causing painful and disabling deformities.
Fortunately, developments in joint reconstruction and replacement have made it
possible to restore hands deformed by crippling arthritis to a nearly normal
appearance and useful function.
Ideally, arthroplasty should produce a joint that is
pain free, mobile, stable, and durable. Four methods of reconstruction for
arthritic joints of the hand have emerged: arthrodesis, resection interposition
arthroplasty, resurfacing joint replacement, and flexible implant resection arthroplasty.
Arthrodesis works very
well for the thumb at the metacarpophalangeal joint level and for the lesser
fingers at the proximal and distal interphalangeal joint level, but lack of
motion is debilitating in the lesser fingers at the metacarpophalangeal joint
level and rarely used.
Resection interposition arthroplasty can improve motion by shortening skeletal structures, lengthening soft
parts, providing new gliding surfaces, and allowing the development of a new
supportive fibrous joint capsule. The chief disadvantage of the procedure in
the metacarpophalangeal joints is the unpredictability of results. Resurfacing
joint replacement has proved successful in knee and hip joints, but early
results in finger joints have been mixed because of dislocation, bone resorption,
and implant loosening. More recently, newer designs are proving useful in
patients with osteoarthritis and early rheumatoid arthritis where the soft
tissue balance is
still relatively normal.
In flexible implant resection arthroplasty, a
flexible silicone implant is used as an adjunct to resection arthroplasty. This
method was devised in 1962 and has been used successfully in several hundred
thousand patients. This discussion emphasizes the techniques of implant
resection arthroplasty.
The basic concept of flexible implant resection
arthroplasty can be summarized as “bone resection + implant + encapsulation =
functional joint.” The flexible implant acts as a dynamic spacer, maintaining
internal alignment and spacing of the reconstructed joint and supporting the
capsuloligamentous system that develops around it. The joint is thus rebuilt
through a healing phenomenon called the “encapsulation process.” Because the
capsuloligamentous system around a new joint is adaptable, a functional balance
of mobility and stability can
be obtained. This allows for realignment of severely dislocated and angulated
joints after the significant bony and soft tissue resection needed in severe
rheumatoid deformities. Postoperative mobilization is tailored to the amount of
instability present after reconstruction; delay in mobilization increases stability.
This is typically acceptable as the flexors greatly over- power the extensors
and prolonged immobilization in extension is rapidly overcome, giving a stable,
mobile grip. Soft
tissue balance is key to preventing the recurrence of deformity and to implant
breakage, dislocation, and failure.
General Considerations
The candidate for arthroplasty must be in good general
condition. Skin cover and neurovascular status must be adequate. The elements
necessary to restore a functioning musculotendinous system and sufficient
bone stock to receive and support the implant must be available. In certain
patients with progressive rheumatoid arthritis who have insufficient bone stock
to support the implant, a simple resection arthroplasty or arthrodesis with a
bone graft is preferable. Surgery is also contraindicated if postoperative hand
therapy is not available or adequate.
Proper staging of the reconstructive procedures is
important in planning the treatment program. Procedures in the upper limbs
should be delayed in patients who also need lower limb reconstruction that will
necessitate the use of crutches. After hand reconstruction, patients should
avoid excessive manual labor and awkward hand weight bearing when using crutches.
The special platform type of crutch is recommended.
In deformities of the metacarpophalangeal joint associated
with severe wrist involvement, the wrist should be treated first. In the
patient with rheumatoid arthritis, tendon repair and synovectomy of tendon
sheaths must precede arthroplasty of the metacarpophalangeal joints by 6 to 8
weeks. If both metacarpophalangeal and proximal interphalangeal joints are
involved, the metacarpophalangeal joint is usually treated first or
simultaneously if only operating on one or two metacarpophalangeal joints. In
swan-neck deformity, the metacarpophalangeal and proximal interphalangeal
joints are reconstructed at the same stage. In boutonnière deformity, the
proximal interphalangeal joint is reconstructed first. Tendon imbalances and
joint misalignment must be corrected. Implant arthroplasty for both the metacarpophalangeal
and proximal interphalangeal joints of the same digit is usually avoided if
possible.
Several procedures can be performed during one operation, depending on the time available. Surgery
for the thumb, proximal interphalangeal and distal inter-phalangeal joints,
wrist, and, occasionally, the elbow joint can often be combined. A limb
procedure should be limited to no more than 2 hours, and an axillary or
supraclavicular block is recommended if the tourniquet time exceeds 112 hours.
Small joints may also be injected with corticosteroids or other agents during
surgery.
Deformities Of Finger Joints
In the normal hand, a delicate balance exists among
the muscles and tendons and the bones and joints through which they interact. The hand has three functional
arches, one longitudinal and two transverse. The proximal transverse arch
crosses the carpal area, with its center at the capitate. The distal transverse
arch is formed by the metacarpal heads and is centered on the head of the third
metacarpal. The digits make up the longitudinal arches, each with its apex at the metacarpophalangeal
joint.
In rheumatoid arthritis, this balance among the muscles,
tendons, and bones is compromised as the inflammatory synovial membrane grows
over the surface of the cartilage, into the ligamentous attachments, and into and around the tendons. The result is capsular
distention, destruction of cartilage, subchondral erosions, loosening of
ligamentous insertions, impaired tendon function, and, finally, joint dis-
organization, subluxation, and dislocation. A break in the longitudinal arch
system causes collapse deformities of the multiarticular structure of the hand,
disturbing the stability and balance necessary for prehension. Use of the hand
in daily activities (functional adaptation) causes further deformity.
Deformities Of Metacarpophalangeal Joint
The metacarpophalangeal joint is a key element in finger
function. This joint not only flexes and extends but also abducts and adducts;
it also has some passive axial rotation. The index finger can pronate up to 45
degrees.
Rheumatoid arthritis commonly involves the metacarpophalangeal
joints, resulting in increased ulnar deviation of the fingers, subluxation of
extensor tendons, and palmar subluxation of joints (see Plate 4-21). The flexor
tendons enter the fibrous sheath at an angle, exerting an ulnar and palmar pull
that is resisted in the normal hand. When the rheumatoid process distends and
weakens the capsule and ligaments of the metacarpophalangeal joint, the forces
generated by the long flexor tendons across the sheath during flexion may
elongate these supporting structures. Resistance to the deforming pull of the
tendons is gradually lost, and the sheath inlet and tendons are displaced in
distal, ulnar, and palmar directions. Eventually, the base of the proximal
phalanx moves ulnarly and palmarly. The intrinsic muscles, which normally form
a bridge between the extensor and flexor systems and provide direct flexor
power across the metacarpophalangeal joint, can also become deforming elements
once the disease has lengthened the restraining structures of the metacarpophalangeal
joint.
Increased mobility of the fourth and fifth metacarpals,
common in rheumatoid arthritis, results from loosening of ligaments at the
carpometacarpal joints and dysfunction of the extensor carpi ulnaris tendon
(ulnar head syndrome). Flexion of the metacarpophalangeal joints increases the
breadth of the transverse arch of the hand, which pulls the extensor tendons in an ulnar direction through the juncture tendons. The
extensor tendon expansions (hoods) are loosely fixed and vulnerable to
disruption. Ulnar subluxation of the extrinsic extensor tendons compromises the
balance of the intrinsic extensor tendons, which in turn increases the tendency
for palmar subluxation and ulnar deviation.
Factors that exacerbate ulnar deviation include (1)
the normal mechanical advantage of the ulnar intrinsic muscles, (2) the asymmetry
and ulnar slope of the metacarpal heads of the index and middle fingers, (3)
the asymmetry of the collateral ligaments, (4) the ulnar forces applied on
pinch and grasp, and (5) the postural forces of gravity. Wrist deformities and
rupture of the extensor
tendons play a secondary role in aggravating the joint disturbances.
Pronation deformity of the index finger is common in
the rheumatoid hand. In the normal hand, pinch between the thumb and index
finger requires a slight supination of the index finger so that the palmar surfaces can meet. In pronation deformity, the less useful lateral surfaces are
opposed. During pinch, pronation deformity is seen in all three digital joints,
but it is more pronounced in the metacarpophalangeal joint. Arthroplasty of
this joint should include reconstruction of the capsuloligamentous and
musculotendinous systems.
Surgery For Metacarpophalangeal Joint
Flexible implant resection arthroplasty of the metacarpophalangeal
joints is carried out for deformities due to rheumatoid arthritis and trauma,
with radiographic evidence of joint destruction too great to support resurfacing
implants or subluxation greater than 25%, ulnar deviation not correctable with
soft tissue surgery alone, and contraction of the intrinsic and extrinsic
musculature and ligamentous system.
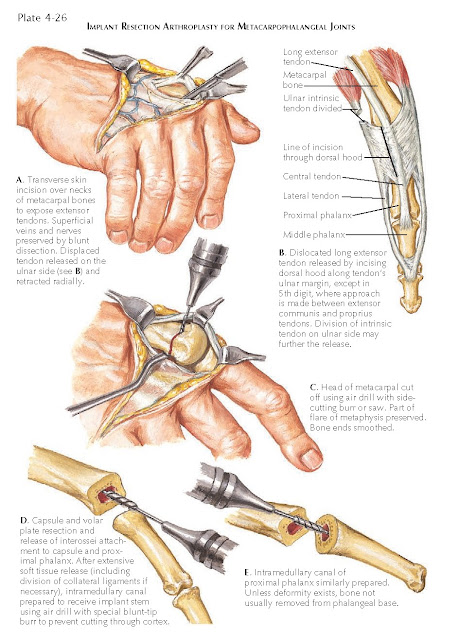
The surgical technique for implant resection arthroplasty
for the metacarpophalangeal joint is shown on Plates 4-26 to 4-28. Soft tissue
release must be complete to obtain an appropriate joint space. The ulnar
collateral ligament is incised at its phalangeal insertion in all fingers; if
severely contracted, it is excised with the palmar ligament (plate). The ulnar
intrinsic tendon, if tight, is sectioned at its myotendinous junction and the
abductor digiti minimi is released.
Reconstruction of the radial collateral ligament is
done for index and middle fingers. The radial collateral ligament and related
structures are reattached proximally to the metacarpal neck and distally to the
proximal phalanx through small drill holes. The radial half of the palmar plate
and the preserved radial capsule are included in this repair. The ulnar edge of
the capsule is sutured to the distally released ulnar collateral ligament.
Sutures are placed before the implant is inserted and tied with the finger held
in supination and abduction. Although the procedure seems to slightly limit
flexion of the metacarpophalangeal joint, this is out-weighed by increased
lateral and vertical stability and better correction of the pronation deformity.
After the procedure, a voluminous conforming dressing,
including a palmar splint, is applied with the metacarpophalangeal joints in 30
degrees of flexion and slight radial deviation. During the postoperative
period, the limb must be elevated. A meticulous postoperative therapy program
is usually started 3 to 5 days after surgery and consists of static splinting
of the metacarpophalangeal
joints for 4 weeks with free movement of the proximal and distal
interphalangeal joints followed by mobilization of the metacarpophalangeal
joints in a radial deviation support brace. Full hand night splinting in a
slightly overcorrected position is used for 6 months.