Eosinophilic
Esophagitis
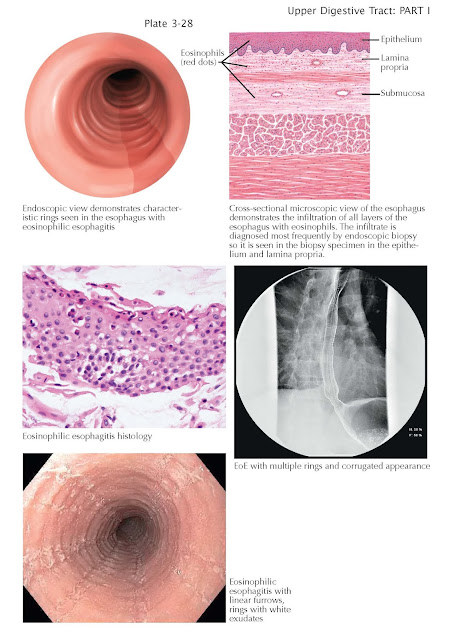
Eosinophilic esophagitis is a newly recognized but common disease
defined by the presence of esophageal symptoms in a patient with esophageal
mucosal eosinophilia not attributable to gastroesophageal reflux or other
causes. It is caused by a combination of an immunoglobulin E response with a
TH2 lymphocyte type of allergic reaction to specific food antigens exposed to
the esophageal mucosa with normal eating.
This in turn leads to chronic
inflammation with dense eosinophilic infiltration. It is more common in men
than women and typically affects children, teenagers, and young adults. Both a
personal and family history of extraesophageal allergies is common. Children
typically have symptoms referable to the inflammatory component of the disease,
including failure to thrive, nausea, vomiting, dyspepsia, and heartburn. With
time, inflammation leads to fibro sis. As a result, stricture formation is
common in this disease, particularly in adults, and dysphagia to solid food
becomes the most likely presenting symptom. Strictures may be of variable
length, from focal distal strictures to uniform esophageal narrowing (small-caliber
esophagus). In addition to strictures, endoscopically, the esophagus has
several characteristic features, including white exudates that represent
eosinophilic abscesses, linear furrows that are longitudinal mucosal tears,
mucosal fragility characterized by easy tearing of the mucosa with minimal
trauma, and esophageal rings with a corrugated appearance due to fibrosis.
Treatment, particularly in adults, is aimed at both control of the inflammation
and dilation of fibrotic strictures. Control of the mucosal eosinophilia may be
achieved through medications such as proton pump inhibitors and
topical corticosteroids. The ideal treatment is identification and avoidance of
the food antigens that trigger the disease in individual patients.
Unfortunately, this is often not practical given the inaccuracy of skin and
blood allergy testing to predict causative food antigens and a lack of reliable
noninvasive testing to monitor the response to multiple trials of food
additions and withdrawals and the multiple foods often identified that need
to be avoided.