PHYTOPHOTODERMATITIS
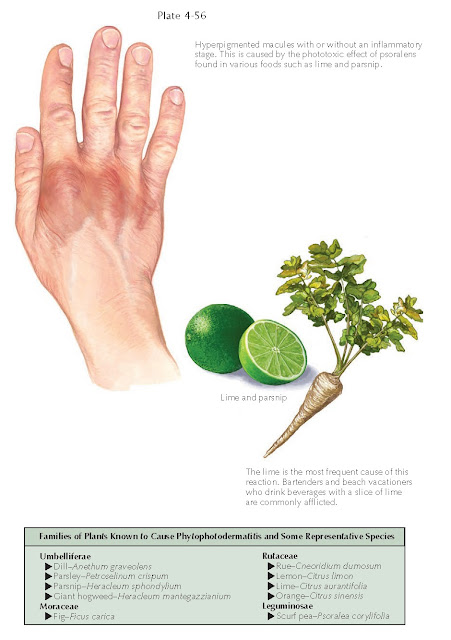
Phytophotodermatitis
is a specific form of phototoxic or photoirritant contact dermatitis. The
offending agent is a plant species from one of a few specific families. This
form of dermatitis has an insidious onset and is typically preceded by little
to no inflammation. This can make the diagnosis difficult for the clinician.
Recognition of the key clinical features and the species of plant involved help
make the diagnosis.
Clinical Findings: Phytophotodermatitis is caused by certain species of plants that come
into contact with the skin. Lone contact with skin is not enough to cause the
inflammatory reaction and subsequent postinflammatory hyperpigmentation: After
exposure to the plant material, there is a time frame during which the exposed
area must be introduced to ultraviolet radiation. It is the plant oils and
resins in combination with the correct ultraviolet source that leads to the
characteristic rash.
The most typical clinical scenario encountered is one
in which the patient comes into contact with a plant that contains a psoralen
compound. One of the most frequently reported causes is the juice of a lime (Citrus
aurantifolia). This plant is categorized within the Rutaceae family. The
Rutaceae family is the most wide spread family of plants that have been
described to cause these types of reactions, with the lime being by far the
most common offender.
Patients often describe the use of a lime in a mixed
drink while vacationing on the beach. The lime juice contacts the skin, and
when the skin is exposed to a specific threshold of ultraviolet light, the
reaction develops. Most often, patients do not complain of any acute symptoms.
If the reaction is severe, burning occurs acutely and the diagnosis is
relatively straight forward.
However, most reactions are subtle and do not appear for a few days to weeks.
Patients typically return home from vacation and notice a subtle
hyperpigmentation around the mouth or scattered on the body where they have
splashed or consciously applied the juice from a lime during sun bathing. The
hyperpigmentation may last for months to years. On rare occasions, a severe
acute reaction occurs with red plaque and vesicle formation.
The many families of plants capable of initiating this
type of reaction all contain the chemical psoralen. Psoralen is a potent
photosensitizer that is used clinically. Once purified, it can be given orally
in the form of psoralen + ultraviolet A light (PUVA) therapy or painted on for
topical PUVA therapy. It is especially helpful for treating refractory hand and
foot dermatoses.
The areas of involvement are typically asymptomatic
and do not show any overt inflammatory features. They appear as hyperpigmented, irregularly shaped macules on the
skin. These spontaneously remit over a few months. Many plants are capable of producing the
reaction.
Pathogenesis: Almost all of
the plants responsible for phytophotodermatitis come from four specific
families: Umbelliferae, Rutaceae, Moraceae, and Leguminosae. These plants all
contain potent photosensitizers in varying concentrations. The chemicals
responsible for photosensitization are the furocoumarins; more specifically, the
psoralens are by far the most important of the photosensitizer chemicals. On
contact, the psoralen penetrates the skin. Subsequent exposure to ultraviolet A
light in the spectrum of 320 to 400 nm causes pyrimidine dimers to form within
the DNA strands, which act to interrupt DNA synthesis. The psoralen and ultraviolet light also can
cause hyperpigmentation (tanning).
Histology: The
pathological features are dependent on the timing of the biopsy. An acutely
inflamed lesion shows a superficial perivascular lymphocytic infiltrate and
dermal edema with apoptotic keratinocytes within the epidermis. Late lesions
show melanophages within the dermis.
Treatment: Acute areas of
involvement can be treated with topical corticosteroid creams. The main issue
in management is dealing with the prolonged postinflammatory hyperpigmentation.
No therapy has been shown to be helpful, but almost all reactions resolve
slowly over time. Care should be taken not to perform a treatment that might lead to
a worse cosmetic outcome.