NEUROREGULATION OF GASTRIC ACTIVITY
The cortical areas that influence gastric motility and secretion are in the posterior orbital gyrus and the adjacent anterior cingulate gyrus. Connections are made, via the medial thalamic nuclei, with the hypothalamus, where fibers descend in the dorsal longitudinal fasciculus, at least as far as the dorsal nucleus of the vagus. Impulses from the anterior hypothalamic region act on the cranial parasympathetic nuclei in the brainstem, and the posterior hypothalamus makes connections with the neurons of the lateral horns of gray matter in the thoracolumbar segments of the spinal cord.
The
efferent innervation of the stomach and duodenum, which governs motility and
secretion, includes the vagus and sympathetic nerves. The vagus nerves, the
principal means of innervation to the stomach, exert augmentative and
inhibitory effects on both motility and secretion through the enteric nervous
system (see below). Gastric tone, motility, and secretory activity are
permanently reduced when the vagus nerves are sectioned, whereas section of the
splanchnic nerve does not essentially alter the functions of the stomach. By
virtue of the autonomy exercised by the intramural enteric nervous system
containing the plexus and nerves, the stomach is able to function adequately
after complete extrinsic denervation (i.e., after bilateral vagotomy and splanchnicotomy).

EXTRINSIC INNERVATION OF STOMACH
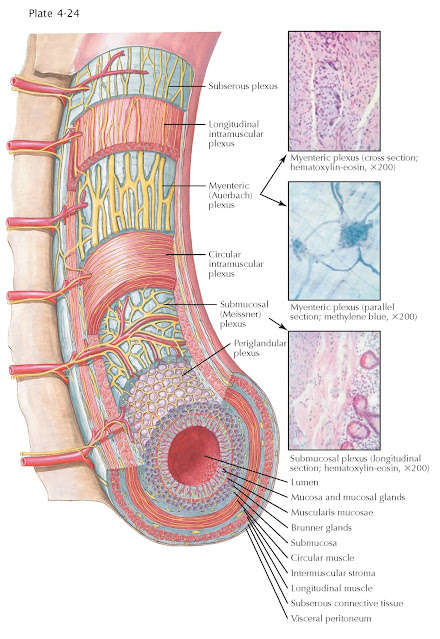
The
vagus nerves and sympathetic nerves help regulate gastric motility by synapsing
on neural cell bodies and projections of the intrinsic intramural enteric
nervous system. The enteric nervous system consists of a system of neurons that
governs the function of the gastrointestinal system. The enteric neurons
synapse on the smooth muscle to reduce or augment gastric contractions. The
gastric contraction frequency is governed by the pacemaker cells in the
stomach, the interstitial cells of Cajal. The neurons of the enteric nervous
system are collected into two types of ganglia, the myenteric (Auerbach)
plexus, which regulates motility, and the submucosal (Meissner) plexus, which
regulates secretion. Myenteric plexuses are located between the inner and outer
layers of the muscularis propria, and
submucosal plexuses are located in the submucosa. The enteric nervous system is
capable of autonomous functions, such as the coordination of reflexes; although
it receives considerable innervation from the autonomic nervous system, it can and does
operate independently of the brain and spinal cord. Because the enteric nervous
system has its own independent reflex activity, it has been described as a
“second brain.”
AFFERENT
INNERVATION
The
gastrointestinal tract is densely innervated to provide information on its
luminal contents, processes regulating digestion and absorption. This
information is collected by intrinsic and extrinsic afferent nerves and regulates
physiologic responses for homeostasis and health. In brief, sensory neurons of
the enteric nervous system activate local responses. Extrinsic afferent nerves
transmit sensory information to the spinal cord or brainstem for further
processing and integration. In general, the extrinsic afferent innervation of
the gut is conducted through the vagus nerve and spinal afferents. The cell
bodies of the vagus afferents are in the nodose ganglion, and mainly project to
the nucleus of the solitary tract. Vagovagal reflexes result in
stimulation of vagal efferents in the dorsal motor nucleus of the vagus nerve.
Examples of vagovagal reflexes are transient lower esophageal sphincter
relaxations and meal-induced gastric accommodation.
The
spinal afferents have cell bodies in dorsal root ganglia. These afferents are
thoracolumbar nerves (with neurons in thoracolumbar dorsal root ganglia and
projections via splanchnic nerves and mesenteric/colonic/ hypogastric nerves)
or lumbosacral nerves (with cell bodies in lumbosacral dorsal root ganglia and
projections via pelvic nerves and rectal nerves to the distal bowel), which
synapse in the spinal cord and send information to the brainstem. Of note, each
region of the gastrointestinal tract receives dual sensory innervation
reflecting functional connectivity for the distribution of extrinsic primary
afferents in these pathways.
The
afferent sensory fibers take their course with the vagus and sympathetic
nerves and mediate the visceral sensations, including nausea, hunger, and pain.
Pain sensations are carried by afferent fibers accompanying the sympathetic
nerves. In contrast to the somatic sensory nerves, the visceral afferents or
their receptors are relatively insensitive to stimuli such as cutting or
burning. The effective stimulus for visceral pain is tension transmitted to the
nerve endings by strong muscular contraction, by distention, or by
inflammation. Normal peristaltic movements of the stomach do not ordinarily
give rise to any sensation, but forceful contractions may be perceived as a
feeling of gnawing and tension or as actual pain in the abdomen, particularly
in the presence of an inflammatory or ulcerative process.
In
addition to the discomfort that the individual locates in the involved viscus,
pain may be felt which is subjectively interpreted as arising in the abdominal
or thoracic wall. The areas to which this referred pain is
ascribed depend upon the distribution of the afferent fibers and their course.
Pain from the stomach is conveyed mainly in the afferents that run in the sympathetic nerves of the
5th to 10th thoracic segments, but the pathways may also extend as
low as the 12th segment. The impulses reach the spinal cord by way of the white
communicating rami and dorsal root ganglia. Within the spinal cord, the
impulses are “transferred” to the neurons of the somatic sensory nerves, with
the result that pain originating in the stomach may be referred to any of the
somatic structures receiving their sensory supply from the 5th to 12th thoracic
segments.