VULVAR VESTIBULITIS
Vulvar vestibulitis is an uncommon syndrome of intense sensitivity of the skin of the posterior vaginal introitus and vulvar vestibule, characterized by progressive worsening, which leads to dyspareunia, vulvodynia, and loss of sexual function. Some estimates place its prevalence at 15% of all women, but significant, disabling symptoms are much less common. Although the median age of occurrence is 36 years, it can occur at any time after the late teenage years. New onset of symptoms is uncommon after menopause.
The cause of vestibular vestibulitis is unknown but there does appear to
be a high degree of association with human papillomavirus, though no causal
link has been established. It has been postulated that the use of oral
contraceptives may increase the risk or severity of vulvar vestibulitis and
that patients with vulvar vestibulitis should switch to other methods of
contraception. Strong evidence for either causation or significant improvement
is lacking. Despite the implication of the term, widespread true inflammation is
not a characteristic of this process.
 |
| Plate 6-11 |
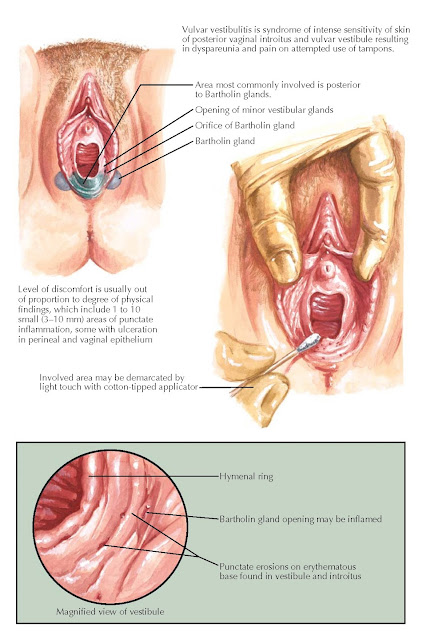
The most common symptom is intense pain and tenderness at the posterior
introitus and vestibule, most often present for 2 to 5 years. (Some authors
suggest that symptoms must be present for more than 6 months before the
diagnosis is made.) Most patients are unable to use tampons (33%) or to have
intercourse (entry dyspareunia, 100%). The appearance of focal inflammation,
punctation, and ulceration of the perineal and vaginal epithelium is common.
On physical examination, punctate areas (1 to 10) of inflammation 3 to 10
mm in size may be seen between the Bartholin glands, hymenal ring, and middle
perineum. Colposcopy of the vulva (using 3% acetic acid) may reveal the
characteristic small inflammatory punctate lesions varying in size from 3 to 10
mm, often with superficial ulceration and acetowhite areas. The Bartholin gland
openings may be inflamed as well. The area involved may be demarcated by light
touching with a cotton-tipped applicator, although the level of discomfort is
often out of proportion to the physical findings. If a biopsy is performed (not
necessary for diagnosis), inflammation of minor vestibular glands may be seen.
Vulvar vestibulitis must be differentiated from cases of vaginismus,
chronic or atrophic vulvitis, hypertrophic vulvar dystrophy, and other vulvar dermatoses, including contact
(allergic) dermatitis.
Initial management includes general perineal hygiene, cool sitz baths,
moist soaks, or the application of soothing solutions such as Burow’s solution
(aluminum acetate, 1 : 40 solution). Patients should be advised to wear
loose-fitting clothing and keep the area dry and well ventilated. Spontaneous
remission may occur in one-third of patients over the course of 6 months.
More specific suggestions include topical anesthetics (lidocaine
[Xylocaine] 2% jelly [or 5% cream] as needed or overnight) and antidepressants
(amitriptyline hydrochloride), which may
reduce pain and itch. Interferon injections may provide relief in up to 60% of
patients but cannot be used in women who are pregnant. (Patients should be
warned that interferon injections are associated with flu-like symptoms and a
clinical response may not be seen for up to 3 months. Patients should abstain
from intercourse during the series of injections.) Refractory disease may
require surgical resection or laser ablation. Surgical therapy is associated with 50% to 60% success rates.




