GASTRIC ELECTRICAL STIMULATION FOR GASTROPARESIS
Gastric electrical stimulation is an emerging treatment for refractory gastroparesis. There are several techniques for stimulating the stomach. First, in gastric electrical pacing the goal is to entrain and pace the gastric slow waves with low-frequency, high-energy, long-duration pulses. Pacing at 10% higher than the basal rate is used to try to accelerate gastric emptying and to improve dyspeptic symptoms. Second, stimulation with high-frequency, low-energy, short-duration pulses has been shown to decrease symptoms but has less effect on gastric emptying; it may affect proximal stomach function and activate sensory afferent nerves to reduce symptoms. Third, sequential gastric neurostimulation of the stomach has been used to entrain gastric slow waves.
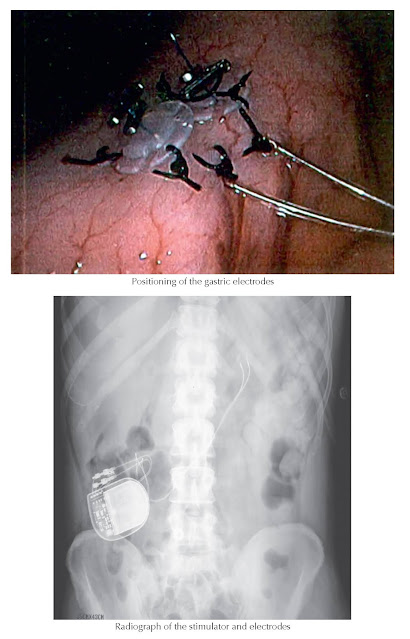 |
| Plate 4-49 |
High-frequency
gastric electrical stimulation at 12 cycles per minute has received
humanitarian approval by the Food and Drug Administration for treatment of
chronic, refractory nausea and vomiting secondary to diabetic or idiopathic
gastroparesis. Stimulating wires are placed into the gastric muscle at the
greater curvature during laparoscopy or laparotomy. These leads are attached to
an electric stimulator (pacemaker), which is placed in a subcutaneous abdominal
pouch. An initial study demonstrated effectiveness in 20 of 26 patients, with a
decrease in nausea and vomiting at 3 and 6 months; gastric emptying of liquids,
but not solids, was improved. In long-term follow-up, 3 of 24 patients
underwent total gastrectomy because of unsatisfactory results, and in 3, the
stimulator was removed because of erosion or infection. A subsequent study
reported on 33 patients with chronic gastroparesis. After implantation, the
electrical stimulator was turned on or off in a randomized, double-blind,
crossover design. Patients felt better when the stimulator was on, although the
decrease in vomiting that occurred was not statistically significant. Long-term
follow-up over 1 year showed a decrease in the mean vomiting frequency from 25
to 6 times per week. In addition, there was an improvement in the overall
quality-of-life score and a mild improvement in gastric emptying. Complications
were infection in 3 patients and electrode penetration of the stomach wall in 1
patient. An open-label study in 25 patients reported an overall improvement
from “severe” to “moderate”
in symptoms of nausea and vomiting of 40%. There was an infection rate of 15%,
requiring removal of the stimulator. Recent reports in both diabetic and
idiopathic gastroparesis with blinded on and off periods of stimulation did not
show significant improvements in symptoms; however, with long-term open-label
stimulation over 1 year, a reduction of symptoms was seen.
Carefully
designed studies are needed to determine the overall effectiveness of gastric
electrical stimulation, which type of patient will likely respond, and the
optimal stimulation parameters. Studies suggest that the patients most likely
to respond are those with diabetic gastroparesis, those with main symptoms of
nausea and vomiting, and those not taking regular narcotic analgesic medications.




