Opioid Use
Disorders
Opioid misuse, abuse, and dependence (opioid use disorders) refer to the pathologic self-administration of substances that activate central mu-opiate receptors, for the purpose of experiencing an altered mental state (euphoria or relaxation), or in the opioid-dependent individual for the purpose of avoiding opioid withdrawal. Naturally-occurring opiates (morphine, codeine) are found in Papaver somniferum poppy pods as a latex sap, opium; heroin is a semisynthetic opioid derived from opium. Prescription analgesics include semisynthetic (e.g., hydrocodone, oxycodone) and synthetic (e.g., methadone, fentanyl) opioids. Both heroin and opioid analgesics may be insufflated or injected to get “high”; other routes include smoking heroin and swallowing/chewing opioid analgesics. Routine toxicology detects only opiates (heroin metabolites), and special gas chromatograph/mass spectrometry (GC/ MS) detection is required for semisynthetic and synthetic opioid analgesics.
According to the 2010 National
Survey on Drug Use and Health, 200,000 U.S. residents age 12 years and older
endorse past-month heroin use, and 5.1 million residents endorse past-month
prescription opioid misuse. Prescription opioid misuse has increased three-
fold in the past decade in conjunction with similar increases in opioid
prescribing and unintentional opioid overdose deaths. Family and friends are
the most frequently reported source of illicit opioid analgesics, con-
tributing to increased youth exposure, high rates (6% past-month prevalence) of
opioid analgesic misuse among 18- to 25-year-olds, and an alarming number of
accidental pediatric ingestions and deaths.
Opioid intoxication may be
recognized by miosis, dysarthria, altered mental state and sedation,
constipation, impaired judgment and slowed reaction time. Recurrent opioid use
results in tolerance to the central effects and progression to physiologic
dependence on opioid-taking to avoid opioid withdrawal. Physiologic
dependence alone is not an opioid use disorder; however, it is when the
individual also experiences preoccupation with obtaining, using, and
recovering from opioid use such that normal social and occupational functioning
is reduced or impaired. Symptoms of opioid withdrawal include mydriasis,
diaphoresis and fever, increased heart rate, abdominal cramps, nausea/vomiting
and diarrhea, lacrimation, rhinorrhea, piloerection, leg cramping, yawning,
insomnia, and anxiety. Although physiologic dependence alone is not
sufficient to define an opioid use disorder, it poses a risk for developing
an opioid use disorder, particularly in vulnerable populations, such as
those with a history of substance abuse, mental illness, or genetic loading for
addiction disorders.
Medical consequences of opioid misuse are many, and risk is proportionate to
the quantity of opioid self- administration, the route of
administration (with injection use carrying the highest probability of
overdose death as well as high rates of blood-borne infectious disease
transmission, especially hepatitis C virus [HCV] and human immunodeficiency
virus [HIV]), and the duration of use (women being more rapidly
susceptible to both medical and social consequences, often referred to as a
“telescoping course”). Overdose mortality is associated with high-dose
opioid use, co-occurring use of alcohol and other sedatives, and injection use.
Injection use is commonly associated with cellulitis and staphylococcal
infection, phlebitis, and endocarditis. Pain is frequently comorbid among
opioid-dependent youth and adults. Social and
legal consequences include loss of employment, domestic violence, and arrest
for drug-related criminal behaviors.
FDA-approved medication
maintenance for opioid use disorders includes
the mu-opiate receptor antagonist naltrexone, the mu-opiate receptor partial
agonist buprenorphine, or the mu-opiate receptor full agonist methadone.
Behavioral therapies without medication maintenance have high failure rates
(relapse to opioid use) in both youth and adults. Optimal
treatment combines medication management with behavioral therapy and participation in self-help programs.
Naltrexone therapy has been limited by poor patient adherence to oral
naltrexone; the recent development of an extended-release injection formulation
that endures 4 weeks may have superior outcomes. Buprenorphine has a
favorable safety and tolerability profile compared with methadone and also
offers office-based access for patients, as opposed to daily monitored dosing
at methadone maintenance clinics. Patients needing
close medical monitoring and more intensive social service supports may benefit
more from the structure of methadone clinics.
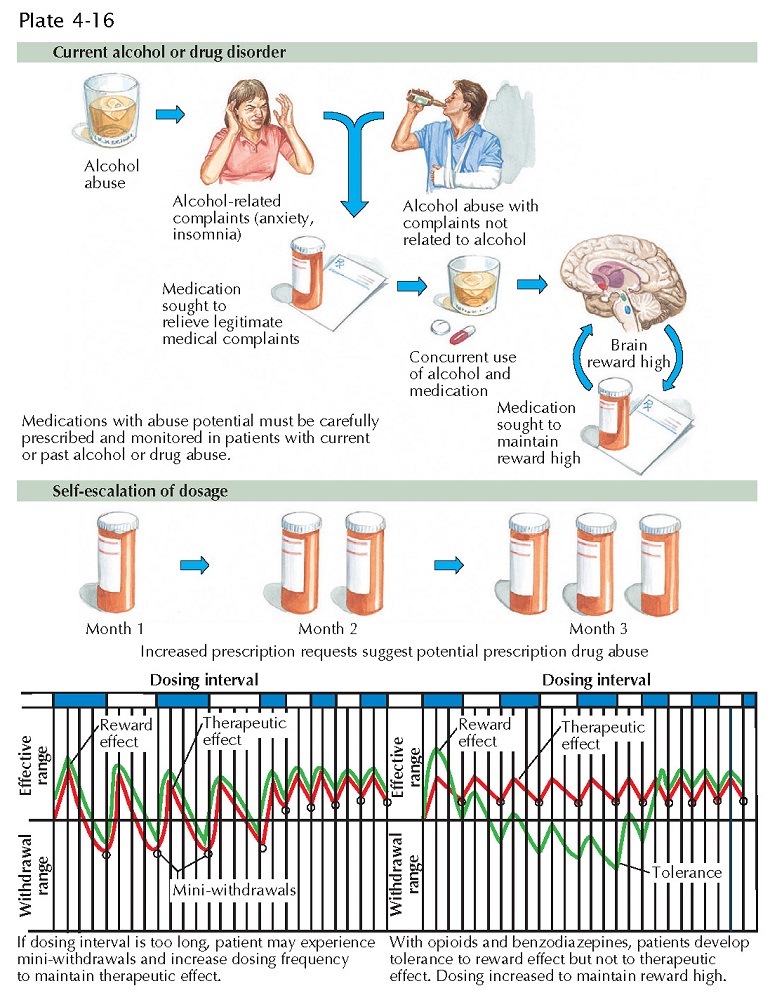
Safe opioid prescribing will prevent diversion of opioid analgesics. Physicians must screen patients for vulnerability to opioid misuse and discuss these risks with patients. Prevention strategies include limiting quantity, using state prescription monitoring services, designated pharmacies and treatment contracts, toxicology, pill counts, and monitoring aberrant behaviors (e.g., “doctor-shopping,” running out early, “lost” or stolen prescriptions). Functional improvement with opioid analgesics must be monitored closely to prevent unnecessary chronic opioid treatment. Patient education on safe storage (lockbox use), safe dosing, and safe disposal are essential and may be remembered using the mnemonic “STOP & DUMP:” secure medication, take only s rescribed, & iscard unused medications and pills.