Gastrointestinal
Tract: Overview And The Mouth
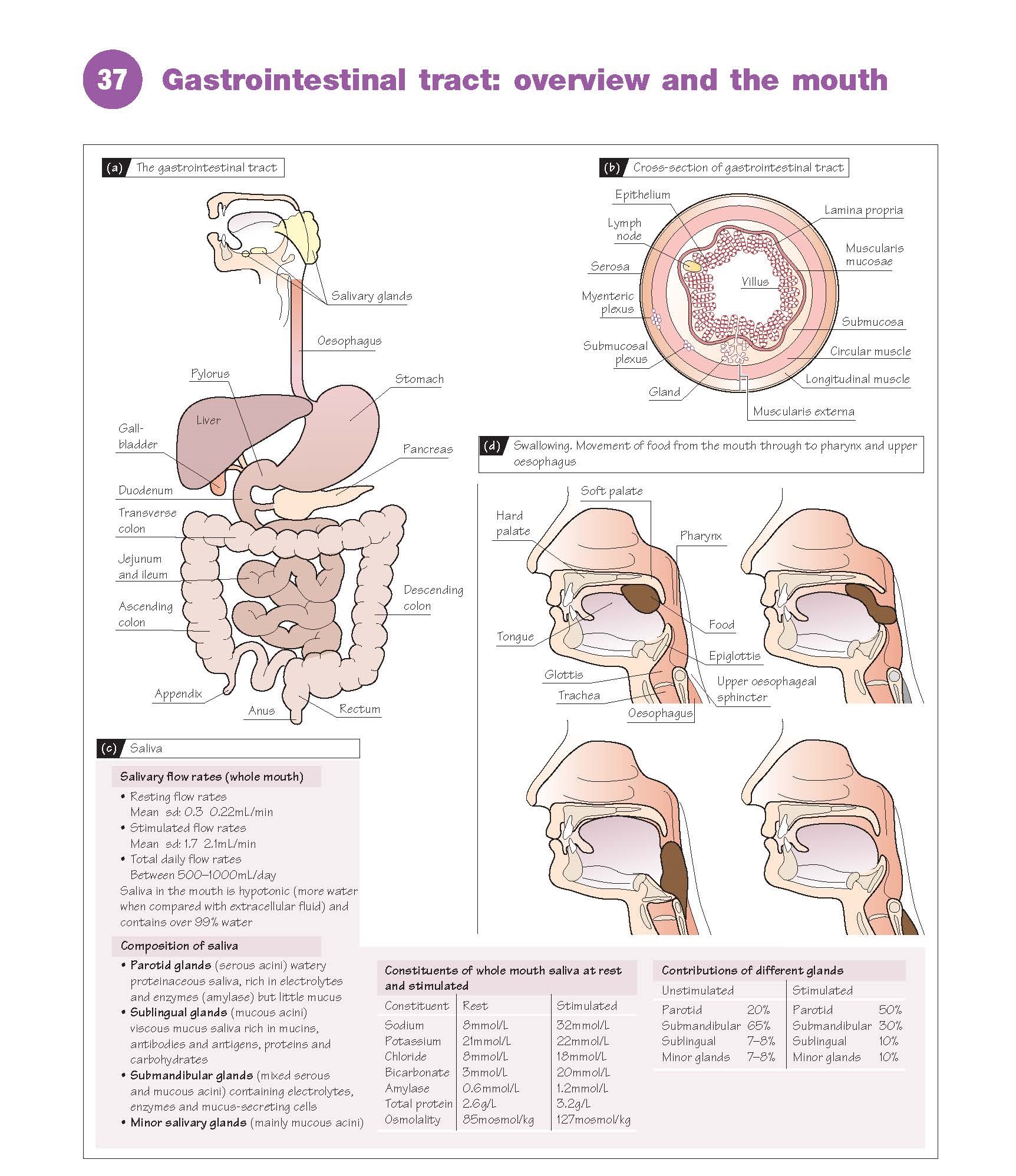
The gastrointestinal
(GI) tract is responsible for the breakdown of food into its component parts so that they can
be absorbed into the body. It is made up of the mouth, oesophagus,
stomach and small and large intestines. The salivary glands,
liver, gallbladder and pancreas are organs distinct from
the GI tract, but all secrete juices into the tract and aid the digestion
and absorption of
the food (Fig. 37a).
Structure
Different regions of the tract are
concerned with motility (transport), storage, digestion, absorption
and elimination of waste, and these functions of the GI tract are
controlled by neuronal, hormonal and local regulatory
mechanisms.
The walls of the GI tract have a
general structure that is similar along most of its length, although this is
modified as function varies. This basic structure is shown in Figure 37b. It
comprises the mucosal layer, made up of epithelial cells (which can be
involved in either the process of secretion or absorption depending on their
location in the GI tract), and the lamina propria, consisting of loose
connective tissue, collagen and elastin, blood vessels and lymph tissue, and a
thin layer of smooth muscle called the muscularis mucosa which, when
contracting, produces folds and ridges in the mucosa. The submucosal layer comprises
a second layer of connective tissue, but also contains larger blood and
lymphatic vessels and a network of nerve cells called the submucosal plexus (Meissner’s
plexus). This is a dense plexus of nerves innervated by the autonomic part
of the nervous system which can function as an independent nervous system – the
enteric nervous system. Below the submucosa is the muscularis externa.
This comprises a thick circular layer of smooth muscle around the GI
tract which, when it contracts, produces a constriction of the lumen. Below
this layer of muscle is another thinner layer of muscle arranged in a longitudinal
manner which, when it contracts, results in shortening of the tract.
Between these two layers of muscle is a second nerve plexus, called the myenteric
plexus (Auerbach’s plexus), which is also part of the enteric
nervous system. The outermost layer of the GI tract is the serosa,
another connective tissue layer covered with squamous mesothelial cells.
Saliva and mastication
The GI tract starts in the mouth,
where food is initially chewed (masticated) and mixed with
salivary secretions. Mastication is the process of systematic mechanical
breakdown of food in the mouth. The amount of mastication necessary in order to
swallow the food depends on the nature of the ingested food: solid foods are
subjected to vigorous chewing, whereas softer foods and liquids require little
or no chewing and are transported almost directly into the oesophagus by
swallowing. Mastication is necessary for some foods, such as red meats, chicken
and vegetables, to be fully absorbed by the rest of the GI tract. However,
fish, eggs, rice, bread and cheese do not require chewing for complete
absorption in the tract.
Mastication involves the
coordinated activity of the teeth, jaw muscles, temporomandibular joint, tongue and other structures,
such as the lips, palate and salivary glands. The forces
developed between the teeth during mastication have been measured to be about
150–200 N; however, the maximum biting force developed between the molar teeth
is almost 10 times this value.
During mastication three pairs of
glands, the parotid, submandibular and sublingual, secrete
saliva. The major functions of saliva are to moisten and lubricate the
mouth at rest, but particularly during eating and speech, to dissolve food
molecules so that they can react with gustatory receptors giving rise to the
sensation of taste, to ease swallowing, to begin the early part of digestion
of polysaccharides (complex sugars) and to protect the oral cavity
by coating the teeth with a proline-rich protein or pellicle that can serve as
a protective barrier on the tooth surface. Saliva also contains immunoglobulins
that have a protective role in avoiding bacterial infections.
Saliva is hypotonic and
contains a mixture of
both inorganic and organic
constituents. The composition varies according to which gland is secreting and
also whether it is resting or being stimulated (Fig. 37c).
The control of salivary
secretion depends on reflex responses which, in humans, have been shown to
be elicited by the stimulation of gustatory (taste) receptors and periodontal
and mucosal mechanoreceptors during mastication. Although it was thought that
olfactory afferent stimulation (smell) also had a general reflex effect on
salivary secretion, it has now been shown that this reflex operates via the
submandibular/sublingual glands and not the parotid in humans. The sight and
thought of food in humans have very little effect on salivary production. The
perception of an increased salivary production is thought to be related to the
sudden awareness of saliva already present in the mouth.
Swallowing
Swallowing occurs in a number of phases. The first phase
is voluntary and involves the formation of a bolus of food by chewing
and tongue movements (backwards and upwards), which push the food into the
pharynx. The remaining phases are not voluntary, but reflex responses initiated
by the stimulation of mechanoreceptors with afferents in the glossopharyngeal
(IX) and vagus (X) nerves to the medulla and pons (brain stem); here, there
is a group of neurones (the ‘swallowing centre’) which coordinates the
complex sequence of events that eventually delivers the bolus into the
oesophagus. The soft palate elevates to prevent food from entering the nasal
cavity, respiration is inhibited, the larynx is raised, the glottis
is closed and the food pushes the tip of the epiglottis over the
tracheal opening, preventing food from entering the trachea. As the bolus
enters the oesophagus, these changes reverse, the larynx opens and breathing continues (Fig. 37d).