Growth: IV Pathophysiology
Clinical scenario
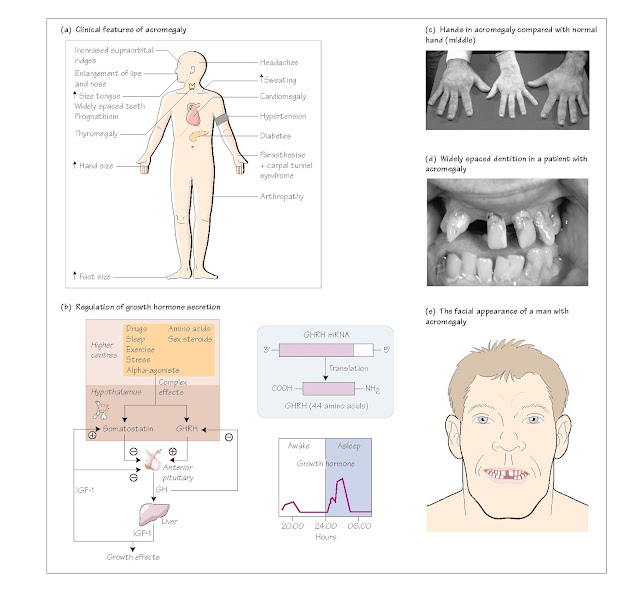
Excess growth hormone (GH) secretion causes the typical syndrome of
acromegaly. Mr SJ was a 53-year-old chef who had generally been well and rarely
went to the doctor. On this occasion he presented to his GP because of aches
and pains in the joints of his hands which were causing a problem with his
work. The GP thought he looked acromegalic and asked him a series of questions
related to his symptoms, following which he established a number of
abnormalities on examination. He referred Mr SJ to the local Endocrine Clinic
where biochemical investigations confirmed the diagnosis of acromegaly. In
particular, his plasma GH level was elevated at 25 mcg/L and failed to suppress
during a glucose tolerance test and his plasma IGF-1 concentration was five
times the upper limit of normal. An MRI scan of the pituitary revealed a
pituitary macroadenoma rising out of the pituitary fossa into the suprasellar
space but not compressing the optic chiasm. He had a good response to pituitary
surgery and subsequent radiotherapy, with resolution of many of the features of
acromegaly. The clinical features of acromegaly are shown in Fig. 12a.
Regulation of growth hormone secretion
Growth hormone (GH) secretion is regulated primarily by the hypothalamus,
which produces growth hormone releasing hormone (GHRH; Fig. 12b). This action
is integrated with the action of a hormone called ghrelin, secreted
mainly by epithelial cells lining the fundus of the stomach. Ghrelin is a potent
releaser of GH from the anterior pituitary gland by binding to pituitary GH
receptors, and is also involved in energy balance (see Chapter 45).
GHRH in humans is a 44 amino acid peptide, which is released into the
portal system and binds to specific receptors on anterior pituitary
somatotrophs to stimulate GH release. The second messenger activated by GHRH is
cAMP, although the IP3 system may also be activated. The hypothalamus also produces
an inhibitory hormone called somatostatin, which inhibits GH release
from somatotrophs. Somatostatin is a 14 amino acid peptide, which also exists
in the hypothalamus in a 28 amino acid form. Both are active in inhibiting GH
secretion, which they do by inhibiting cAMP production. Both GHRH and
somatostatin have been localized to the arcuate nucleus (see Chapter 5). GH is
released in a pulsatile fashion with the major peak in secretion occurring
about one hour after the onset of sleep. In adults, circulating GH levels are
low or undetectable for most of the
day with intermittent bursts of secretion being observed. Somatostatinergic
tone is felt to be the most important determinant of production of a GH peak –
troughs in somatostatin production being associated with a GHRH peak and
subsequent GH release. The physiological feedback control of GH release is
mediated by insulin-like growth factor (IGF- 1), which stimulates somatostatin
secretion from the hypothalamus and inhibits GH secretion directly.
Pathophysiology of growth hormone secretion
GH deficiency
Causes of GH deficiency are either genetic, resulting in short stature in
children (Chapter 10) or acquired, leading to the adult GHD syndrome. GH
deficiency is treated by replacement with human growth hormone (hGH).
Originally extracted from post- mortem human pituitaries, nowadays hGH is
synthesized using recombinant DNA techniques, which obviates the hazards
inherent in using human-derived material, which carries with it the danger of infection.
GH excess
Excess secretion of GH results in acromegaly in adults (see
Clinical scenario) and gigantism in young adults if affected before
fusion of the bony epiphyses. The usual source of excess GH secretion is a
pituitary adenoma. Rarely, ectopic neuroendocrine tumours secreting GHRH occur,
either in isolation or as part of the MEN 1 syndrome (Chapter 50). Acromegaly
results in a coarsening of the facial features and of the soft tissues of the
hands (Fig. 12c) and feet. Exaggerated growth of the mandible (lower jaw)
occurs, resulting in a characteristic facial configuration (Fig. 12d and e).
There is hypertrophy of connective tissue of the kidney, heart and liver, and
the patient’s glucose tolerance is lowered by up to 50%, resulting in diabetes
in about 10% of patients with acromegaly. Other symptoms include headaches,
sweating, renal colic due to nephrolithiasis and arthralgia. A diagnosis of
acromegaly is confirmed by the failure of elevated GH levels to suppress during
an oral glucose tolerance test, coupled with elevated serum IGF-1
concentrations.
The treatment of choice for acromegaly is surgical removal of the
pituitary adenoma, plus or minus adjunctive radiotherapy or medical treatment
with somatostatin analogues or dopamine agonists. Untreated, acromegaly is
associated with increased mortality
from cardiovascular disease and cancer.