Melanocytic Nevi
There are numerous types of melanocytic nevi,
including the benign congenital melanocytic nevi, the blue nevi, and the common
acquired melanocytic nevi. Atypical and dysplastic nevi are discussed with
melanoma in the section on malignant growths. Evaluation of melanocytic nevi is
one of the dermatologist’s most common and important tasks. Every patient who
enters a derma- tologist’s office should be offered the opportunity to have a
full-body skin examination, specifically evaluat- ing melanocytic nevi for any
signs of malignant transformation and or de novo melanoma production. The
importance of evaluating melanocytic nevi is to screen for melanoma. Melanoma
is a life-threatening skin cancer that, if discovered early, can be cured.
Different types of melanocytic nevi have varying rates of malignant
transformation, and it is critical for the clinician to be aware of those nevi
that are likely to be encountered on a daily basis.
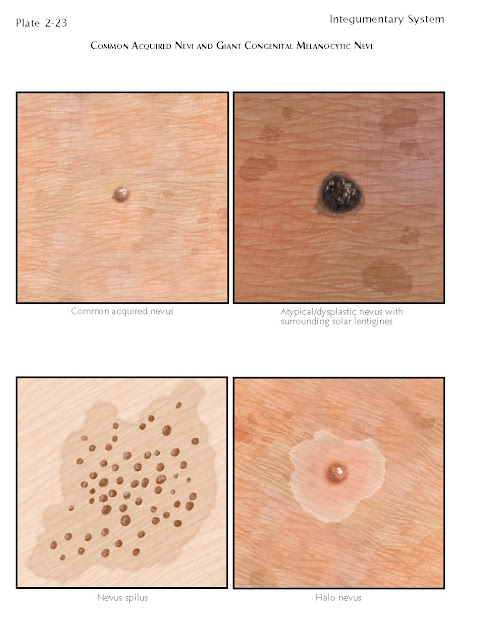
Clinical Findings: Melanocytic nevi can be classified both clinically
and histopathologically. The common acquired melanocytic nevus is a clinical
diagnosis, and if the lesion is biopsied, it may show some evidence of atypia
or dysplasia of melanocytes. It is for this reason that a universally accepted
classification of melanocytic nevi has yet to be adopted.
Benign melanocytic nevi are extremely
common. Virtually all humans have some form of these growths on their body.
Common acquired melanocytic nevi are universally found and can have varying
morphologies. They affect males and females equally. They are uncommon at birth
but increase in number over the first 4 decades of life, after which the number
typically stabilizes. As one ages, the nevi tend to slowly involute. They can
be macular or papular in appearance. Most are uniform and symmetric in size and
color. They can be flesh colored or slightly brown in coloration. They tend to
grow proportionally as a child grows or as an adult gains weight. They also can
become slightly larger and darker during pregnancy.
There is a risk for malignant
degeneration into mela- noma, and changes in color, size, symmetry, or border
should be assessed. Nevi that become symptomatic, especially pruritic, and nevi
that spontaneously bleed should be evaluated and biopsied appropriately.
Blue nevi are unique benign
melanocytic tumors that have a characteristic clinical and histological
pattern. These nevi tend to be small, to be located on the dorsal aspect of the
hands or feet, and to have a bluish to blue-gray coloration due to their
location within the dermis. The blue color is believed to result from the
Tyndall effect. This is a process by which various wavelengths of light are
absorbed preferentially, and the reflected light or color that is seen depends
on the material and depth of the substance being illuminated. Blue nevi share
similar histological characteristics with the nevus of Ota, nevus of Ito, and
Mongolian spots. However, the clinical appearance is so different that these
lesions are not considered in the differential diagnosis of a blue nevus.
Blue nevi can occur at any age, and
they appear equally often in men and in women. They typically manifest as small
(2-5 mm), oval or round macules or papules. They are well circumscribed with
nice, distinct borders. They are commonly located on the dorsal aspect of the
hands and feet but have been reported to occur anywhere, including the mucous
membranes. They are frequently biopsied because of their unusual coloration. They
are small and usually can be removed easily with a punch biopsy that is 1 mm
larger than the lesion. Patients often give a history of having been stabbed
with a pencil during childhood and believe that the lesion is a graphite
tattoo. This occasionally is the case, but most of these lesions are actually
blue nevi. Malignant transformation of blue nevi is extremely rare.
Multiple blue nevi can be seen in the
Carney complex, also known as the NAME or LAMB syndrome. This complex of
clinical findings includes multiple blue nevi, lentigines, ephelides, myxomas,
atrial myxomas,testicular tumors, pituitary tumors, psammomatous melanotic
schwannomas, and adrenal tumors. This is a rare syndrome that has been
determined to be caused by a genetic defect in the gene PRKAR1A. This is
a tumor suppressor gene that encodes a protein kinase A subunit.
Congenital melanocytic nevi can be
divided clinically into distinct subtypes based on size (small, medium, and
giant). Small congenital nevi are the most common type; they are defined as
those nevi smaller than 2 cm in greatest diameter. These nevi occur with equal
frequency in males and females and have no race predilection. Some authors
estimate their prevalence at about 1% of the population. These nevi are
typically described as well-defined macules, papules, or plaques. They are
hyperpigmented compared with the normal surrounding skin. They are almost
always uniform in color and symmetric. Over time, some 50% develop terminal
hair growth within the nevi. The risk of malignant trans- formation in these
small congenital nevi is low and approaches that of the common acquired
melanocytic nevi. Melanoma can arise in these nevi at any point in the
patient’s life but usually after puberty.
Medium-sized congenital melanocytic
nevi are defined as those that have a diameter between 2 and 20 cm. They have
the same risk of malignant transformation as small congenital nevi. They occur
equally in males and females and can be seen in about 1% of the population.
They can occur anywhere on the body.
Giant or large congenital melanocytic
nevi, also known as “bathing trunk” nevi, are important clinically in many
ways. First, they have an increased risk of malignant transformation. This
transformation can be difficult to discern clinically until the lesions are
quite large. Most melanomas develop in a dermal or subcutaneous location, which
make them difficult to assess clinically. Melanomas typically occur before
puberty, and they have been reported to occur in as many as 15% of giant congenital
nevi. The risk of malignant transformation is higher in axial nevi than in
acral nevi. For this reason, these lesions are treated more aggressively, and
patients with large congenital melanocytic nevi need lifelong, frequent routine
follow-up. These nevi occur equally in men and women and in any racial group.
They affect the truncal region more often than any other region of the body.
The significant finding of
neurocutaneous melanosis occurs at a higher rate in patients with large
congenital nevi of the trunk. These nevi almost always occur over the majority
of the trunk, and they can have any number of satellite melanocytic nevi.
Patients with large truncal congenital melanocytic nevi should undergo magnetic
resonance imaging (MRI) of the nervous system to evaluate for neurocutaneous
melanosis. Patients with neurocutaneous melanosis are at a high risk (almost
50%) for development of leptomeningeal melanoma, which is almost always fatal.
A multidisciplinary approach to care for these patients is required, including the patient’s pediatrician, dermatologist, neurologist, and neurosurgeon.
Histology: In common acquired melanocytic nevi, the
melanocytes are arranged symmetrically in a lateral fashion. They are arranged
in nests. The nested mela- nocytes do not have the typical dendritic appearance
of normal melanocytes found within the stratum basalis. They are round and
uniform in shape and show increasing maturation with depth in the dermis.
Maturation of nevi cells implies a decrease in the ratio of nuclear to
cytoplasmic volume and an overall decrease in the size of the melanocytes. The
melanocytes are still uniform in size and shape at various depths within the
dermis; they are not symmetric vertically. Many forms are seen histologically.
Based on the location of the melanocyte nests, they can be classified as
junctional, intraepidermal, dermal, or compound nevi. A junctional nevus has
its nests arranged along the basement membrane zone, whereas a compound nevus
has epidermal and dermal nests.
Blue nevi are located entirely within
the dermis. These nevi are made of melanocytes that resemble dendrites. The
dendritic processes contain melanin pigment, and this pigment is responsible
for the coloration of the lesion. Collagen is interwoven between the dermally
located melanocytes. Melanophages are almost always seen in and around the
lesion. A grenz zone is sometimes appreciated above the melanocytic lesion.
Numerous histological subtypes of blue nevi have been described, including the
dendritic blue nevus (common blue nevus), amelanotic blue nevus, cellular blue
nevus, and epithelioid blue nevus.
Small, medium, and large congenital
nevi all show the same histological characteristics, and they cannot be
distinguished on pathological evaluation. The major criteria used to separate
congenital nevi from other types of nevi are size and location. The nests are
found deep within the dermis and can also be found within the subcutaneous
tissue, fascia, and underlying muscle. Infiltration of muscle is unusual and is
more likely to be seen in large congenital nevi. The nests of nevus cells
accumulate around adnexal structures and are frequently seen juxtaposed to
hair follicles, sebaceous glands, and eccrine glands. The melanocytes can penetrate the arrector pili muscles. The nevus cells show proper maturation and
are uniform in appearance.
Pathogenesis: There are many conflicting theories as to the
pathogenesis of common acquired melanocytic nevi and blue nevi. Some think that
there is an abnormal migration of melanocytes embryologically, whereas others
believe that stem cells are located within the dermis or epidermis and
melanocytes migrate upward or downward to form the nevi. Perhaps a combination
of these processes occurs, but no definitive pathogenic mechanism has been
universally accepted.
Congenital melanocytic nevi are
thought to be caused by an embryological malfunction of melanocyte migration.
The precise mechanism that causes the disrupted or abnormal migration of
melanocytes into the involved areas has not been determined. Migration in these
cases is believed to be controlled by a complex but abnormal growth and
regulatory signaling pathway.
Treatment: Common acquired melanocytic nevi do not need to be
treated. They can be removed by various means for cosmetic purposes. Shave
removal and punch biopsy removal are two highly successful techniques.
Elliptical excision should be reserved for larger lesions in areas where the
scar can be camouflaged. Only highly skilled physicians should consider
removing pigmented lesions with laser therapy, because there is no tissue left
for histological evaluation.
Blue nevi are easily removed by punch
biopsy or elliptical excision. They are often removed for cosmetic reasons, and
a small excision gives an excellent cosmetic result.
Removal of small and medium congenital
nevi should be done with surgical excision. This removes the entire lesion and
allows for pathological evaluation. Most of these small and medium congenital
melanocytic nevi can be observed over time and removed if there are changes.
Serial photographs are invaluable in monitoring these nevi for changes. Some of
these lesions occur in cosmetically sensitive areas, such as the face, and patients
should be referred to a plastic surgeon for evaluation. The social and
psychological well-being of the child can be enhanced by having a disfiguring
congenital nevus removed.
Large congenital nevi present the
biggest treatment difficulty because of the high rate of malignant
transformation. If possible, serial excisions to remove large nevi are the best
option. Tissue expanders are often used to help decrease the need for skin
grafting. The goal should be 100% removal, although in some cases this is not
feasible. If the nevi cover 10% to 30% or more of body surface area, they
become almost impossible to remove. In these cases, as in all the others, the
importance of lifelong surveillance needs to be taught to the parents, the
afflicted individuals, and the participating physicians. The goal in these
cases is to biopsy and remove any changing areas of the nevi in an effort to
prevent metastasis if a melanoma were to develop.