Invasive
squamous cell carcinoma accounts for 80% of cervical malig- nancies. Unlike the
remainder of the reproductive tract cancers, which are more prevalent in
industrialized countries, cervical cancer ranks second in cancer mortality in
developing nations. Virtually all cervical cancers are associated with the
human papillomavirus (HPV), which is the most common sexually transmitted
infection. Squamous cancer of the cervix is unique in that it is a preventable
disease when vaccina- tion, proper screening and treatment are available and
employed.
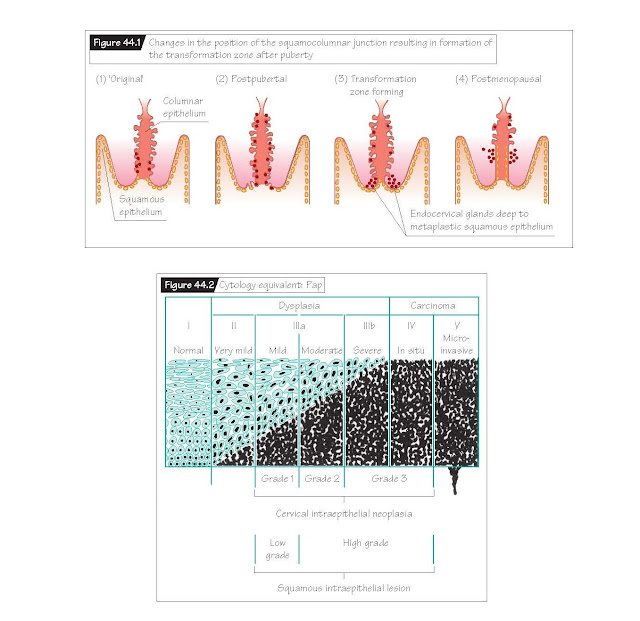
Like
prostatic cancer in men (Chapter 41), cervical cancer typically arises from a
precursor lesion, cervical intraepithelial neoplasia (CIN). CIN is asymptomatic
and appears to precede invasive carcinoma of the cervix by 5–15 years. Almost
all cervical cancer arises in the transformation zone (squamocolumnar junction)
of the cervix. Here, the columnar, glandular epithelium of the endocervix meets
the squamous epithelium of the ectocervix. The anatomic location of the squa-
mocolumnar junction changes in response to a variety of factors and is
different in young postpubertal girls when compared with postmeno- pausal women
(Fig. 44.1). In older women, the transformation zone may be high in the
endocervical canal. This makes the early diagnosis of cervical neoplasia more
difficult.
Cervical
carcinomas can spread in any one of four ways: (i) directly into the vaginal
mucosa; (ii) directly into the myometrium of the lower uterine segment; (iii)
into the paracervical lymphatics and from there to the obturator, hypogastric
and external iliac lymph nodes; and (iv) directly into adjacent structures such
as the bladder anteriorly, the rectum posteriorly, or the parametrial tissues
and pelvic sidewalls laterally. Lymphatic invasion can occur even when cervical
tumors are still small. Hematogenous spread and distant metastases are usually
very late manifestations of the disease.
Surgical
treatment is used for early-stage cervical cancers. A combination of radiation
and chemotherapy is used for patients with advanced disease and in those who
are poor surgical candidates.
Epidemiology of cervical cancer
The
association of sexual activity with cervical cancer was first identified over
150 years ago when it was noted that the disease was rare in nuns and frequent
in prostitutes. Subsequent epidemiologic data have identified the onset of
sexual activity in adolescence and multiple sexual partners as high-risk
characteristics for cervical cancer. Its incidence is higher in low-income
women but this effect is not inde- pendent of early sexual activity and
multiple sex partners. Smoking is an independent risk factor for the
development of cervical cancer. Characteristics of a “high-risk” male partner
include men whose previ- ous partner developed cervical cancer, who themselves
develop penile cancer or who have not had a circumcision.
Epidemiologic
data suggesting that cervical cancer behaves like a sexually transmitted
disease led to identification of HPV as the causative agent. Although it has
been identified in over 99% of all cervical cancers, HPV infection of the
cervix appears necessary but not sufficient for the development of cervical
cancer. This distinction is important as cervical infection with HPV is very
common; however, the majority of these infections are transient. Persistent
infection with an oncogenic type of HPV confers an increased risk of developing
cervical cancer.
Pathogenesis of squamous cell
neoplasia of the cervix
Because the
cervix is so physically accessible, the pathogenesis of cervical neoplasia has
been studied extensively. Pathogenesis clearly involves exposure of a
vulnerable tissue (the transformation zone) to carcinogens.
The
squamocolumnar junction is one of six epithelial boundaries present within the
lower genital tract. The position of the squamoco- lumnar junction is affected
by the hormonal and anatomical changes of puberty, pregnancy and menopause
(Fig. 44.1). Prior to puberty, the squamocolumnar junction is at the level of
the external cervical os (Chapter 9). With puberty, estrogen-induced changes in
the shape and volume of the cervix carry the squamocolumnar junction out onto
the anatomic ectocervix. This repositioning exposes tissues previously found in
the lower endocervical canal to the vaginal environment. The exposure of the
simple mucin-secreting epithelium to the acidic vaginal milieu induces a
chemical denaturation of the villus tips of the columnar epithelium. The
reparative process that follows eventually produces a mature squamous
epithelium. After menopause, the squamocolumnar
junction retreats to a position high within the endocervical canal.
HPV is a DNA
virus that causes epithelial lesions in the skin, cervix, vagina, vulva
(Chapter 47), anus and oropharynx. More than 100 types of HPV have been
identified to date. The HPV infections affecting the genital tract are
classified according to their oncogenic potential. The highest risk HPV
genotypes are 16 and 18, which have been detected in 65% of cervical cancers.
Cervical infection with HPV is very
common –
80% of all sexually active women will have at least one infection with HPV;
however, the majority of these infections are transient. The average duration
of infection is 8 months, and 90% of HPV infections in young women will clear
within 2 years. It is thought that the local immune response of the host is
primarily responsible for HPV clearance; only persistent (greater than 6–12
months’ duration) HPV infection puts the cervix at risk for changes that could
develop into cancer. Typically, HPV infection persists for greater than 10
years before causing carcinogenesis. Women with an impaired immune system,
such as HIV-infected women, have high rates of persistent cervical HPV infections
and cervical neoplasia.
Cervical
intraepithelial neoplasia (CIN) is the term used to encompass all premalignant
epithelial abnormalities of the cervix. It has replaced an older terminology
that used the terms “dysplasia” and “carcinoma in situ” of the cervix. CIN,
although divided into grades, is actually a single neoplastic continuum.
The designations CIN1, 2 and 3 reflect the extent of the cellular aberrations
within the cervical epithelium (Fig. 44.2). For instance, in CIN1, the lower
one-third of the epithelial cells (closest to the basement membrane) lack
evidence of differentiation or maturation. This exit from the normal
differentia- tion pathway signals neoplastic transformation.
Screening tests for cervical cancer
The cervical
smear or Pap test (named after Dr. George Papanicolaou who developed the
test) was designed as a screening test to detect squamous cell abnormalities.
Its success is based on the fact that the nuclear abnormalities of neoplastic
cervical cells are present in samples that are scraped or exfoliated from the
surface of the cervix. In countries where cervical cancer screening with Pap
testing is routinely performed, the incidence and mortality rates of cervical
cancer have both decreased by 70%. It is likely that the treatment of premalignant
lesions and the finding of earlier stage cervical cancers have contributed to
the decreased incidence and mortality of cervical cancer. HPV tests of the
cervix can be used as an adjunct to cervical cytol- ogy screening for women
aged 30 years and over. HPV testing for primary screening of younger women is
not recommended because of the high rates of transient HPV infections that
would be detected. The benefits of adding HPV testing include: (i) a reliable,
readily reproducible measure of the risk of disease; (ii) a high negative
predictive value with a single test that allows prolongation of the screening
interval; and (iii) increased sensitivity (although lower specificity) compared
with cervical cytology in the detection of CIN2–3.
Prophylactic HPV vaccination
Two
prophylactic HPV vaccines based on virus-like particles (VLPs) have been
developed. Both provide protection against HPV types 16 and 18 – the causative
agent for approximately 65% of cervical cancers worldwide. HPV vaccines prevent
the development of HPV 16 and 18 infections, HPV 16 and 18 associated CIN2 or
3, adenocarcinoma in situ and invasive cervical cancer, with 98%
efficacy in young women without prior HPV 16 or 18 infection. Vaccination is
recommended for girls who are not yet sexually active as HPV infections rates
are very high among adolescents. Interestingly, the mechanism of action of
these vaccines is not well understood as the primary mode of natural immunity
to HPV is a local immune response and not a systemic response.
Cervical adenocarcinoma
Adenocarcinoma
of the cervix is much rarer than squamous cell lesions. It occurs most often in
women during the reproductive years and is frequently associated with HPV type
16 or 18. Although adeno- carcinoma in situ is thought to be the
precursor lesion of invasive cervical adenocarcinoma, the timing of progression
from precursor to invasion is not well-defined. Cervical cytology does not
reliably detect adenocarcinomas but may detect concomitantly present cervical
squamous neoplasia; HPV testing should have improved sensitivity for the detection
of adenocarcinomas.