Burns
Burns are a
common problem, but the vast majority are relatively minor. Serious burns
undergo initial assessment and resuscitation as per any trauma (Chapter 8).
History
Eye-witness
accounts from ambulance personnel or witnesses are helpful in assessing the
risk of associated problems such as trauma (jumping from buildings) or blast
injuries. Patients trapped in confined spaces may have inhalation injuries or
exposure to toxic gases such as carbon monoxide and cyanide.
AMPLE
history (Chapter 9) and tetanus immunisation status are important.
Resuscitation
The patient
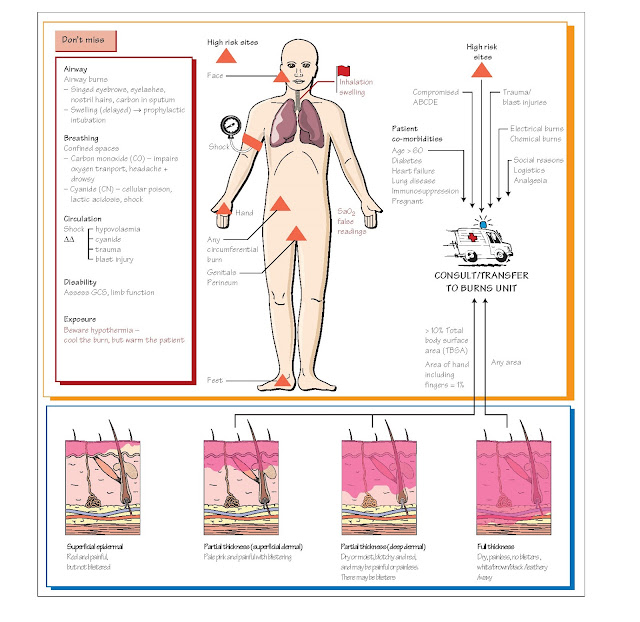
• Airway: look for signs of inhalation injury: carbon/soot in nostrils or mouth,
singed eyebrows/eyelashes/nostril hairs, facial burns, and any orophayryngeal
redness or swelling, change in voice or stridor.
Upper airway
burns require urgent prophylactic intubation with an armoured (crushproof)
endotracheal tube, as the face and oropharynx swell massively within a few
hours.
•
Breathing: oxygen via a reservoir mask for all patients.
•
Circulation: two large-bore intravenous cannulae, through burned skin if necessary.
Take blood for FBC, U+E, LFTs (liver function tests), CK (creatine kinase),
group and save, clotting.
The burn
•
Stop the burning: remove clothes, chemicals, initial cool water.
• Treat the pain: large doses of morphine are required for large burns. Pain is caused by
air movement over the burn: clingfilm can help analgesia.
• Secondary survey: look for signs of other injuries, e.g. jumping from
a height, blast injuries. Look for burned areas needing escharotomy (incision
of the burn to prevent constriction of underlying tissues), e.g. limbs with
circumferential burns, thorax.
• Measurement of the burn: size of patient’s hand including fingers = 1% TBSA (total body surface area).
•
Intravenous fluids: see below.
•
Tetanus: tetanus immunoglobulin should be given according to local protocol.
•
No antibiotics: antibiotics should not be given routinely.
•
Investigations: bedside urinalysis, ECG; blood tests as above, chest X-ray.
•
Transfer: consider the need to contact a burns unit.
• Keep warm: although initial cooling may be helpful, burns patients are at risk of
hypothermia. Wrap burned areas in clingfilm and place patient in dry, sterile
sheets. Use warm air heating blanket and warmed humidified oxygen to minimise
heat loss.
Complicated
or non-thermal burns such as those from bitumen, chemicals, and electrical
injuries require expert assessment, as the injury may be more extensive than is
immediately apparent.
Intravenous fluids
Widespread
capillary damage results in massive loss of intravascular fluid and protein.
Give warmed crystalloids using the Parkland formula and monitor urine output.
Minor burns
These can be
dressed in many ways according to local practice including:
•
Dry non-adherent dressings.
•
Gel-based hydrocolloid dressings.
•
Adhesive woven dressing direct to skin.
•
Silver sulphasalazine cream (never on face). Discharged patients need:
• A clear management plan including analgesia, community support and medical
and nursing follow-up.
• In elderly patients consider an Occupational Therapy assessment to
identify risks of further injury.
Carbon monoxide and cyanide
poisoning Carbon monoxide poisoning occurs in fires, but is also a mode of suicide;
it is most commonly caused by inadequately ventilated heating. Symptoms are
often non-specific, e.g. headache, nausea and vomiting that resolves when out
of the house.
Carbon
monoxide has a much higher (200 x) affinity for haemoglobin than oxygen. Oxygen
saturation monitors cannot differentiate between carboxyhaemoglobin (COHb) and
oxyhaemoglobin, so give falsely normal readings. COHb is measured in blood gas
analysers: venous blood may be used. Smokers and city dwellers may have COHb
levels of up to 10%.
Treatment of
COHb levels above 10% is by 100% oxygen, which reduces the half-life of COHb
from 240 to 75 minutes. Hyperbaric oxygen has not been shown to give additional
benefit.
Cyanides are
formed by furniture burning in enclosed spaces. Diagnosis and treatment is described
in Chapter 47.
Electrical burns (including
lightning) Electricity follows the path of least resistance, which tends to be
nerves, blood vessels and, to a lesser extent, muscle. Skin burns – entry and
exit points – may appear relatively minor, and the full extent of electrical
burns may not be apparent immediately.
High-voltage
(> 600 V) injuries produce
heat injury in underlying tissues and can cause cardiac damage and compartment
syndrome. If a patient hit by lightning makes it to hospital, their chances of
survival are good. Admit all patients with high-voltage burns, but patients
exposed to domestic electricity (110–220 V AC) may be discharged if they have a
normal ECG and no evidence of burns or systemic injury.
Chemical burns
Seek early
expert advice with chemical burns. Both alkaline and acid substances can burn
the skin: alkalis such as drain cleaner and cement are generally worse as acids
tend to precipitate proteins, preventing deep burns. Water is used until pain
resolves and pH is neutral.
Hydrofluoric
acid burns deeply and painfully, binding calcium ions, causing local and
systemic hypocalcaemia. Treatment is by local or systemic calcium gluconate,
which can be given as a gel, injection into the wound, intravenously (like
IVRA) or intra-arterially.