Axilla Anatomy
The axilla is the space between the
root of the upper limb and the chest wall. It is traversed by the principal
vessels and nerves that pass between
the upper limb and the root of the neck. The shape and size
of the axilla vary according to the position of the shoulder joint but when the
limb is in the anatomical position the axilla is shaped as a truncated pyramid
with a narrow apex (inlet) superiorly, a broad base and three walls (Fig.
3.12).
 |
Fig. 3.14 Structures that pass above
pectoralis minor in the anterior wall of the axilla. Pectoralis major and
fascia around pectoralis minor have been removed.
Walls
The upper ribs and intercostal spaces,
covered by serratus ante- rior, form the medial wall (Fig. 3.15), which is
convex laterally. The anterior wall consists of pectoralis major overlying
pectoralis minor and subclavius (Figs 3.14 & 3.16), while the posterior wall is formed by
subscapularis, teres major and latissimus dorsi. The muscles of the anterior
and posterior walls converge on the humerus (Fig. 3.15) so that the axilla is
limited laterally by the narrow intertubercular sulcus of the humerus. The base
of the axilla, convex upwards, is formed by fascia passing between the inferior
margins of the anterior and posterior walls. The triangular apex of the axilla
provides continuity between the root of the neck and the upper limb and is
bounded by the clavicle, the superior border of the scapula and the first rib (Fig.
3.13).
The axilla contains the axillary
artery and its branches, the axillary vein and its tributaries, parts of the
brachial plexus and the axillary lymph nodes.
Coracobrachialis and the short and
long heads of biceps brachii traverse the axilla. In addition, the tail of the
breast usually enters the axilla. All these structures are embedded in loose
fatty connective tissue (Fig. 3.15).
 |
Fig. 3.15 Transverse section showing (left)
the walls and (right) the contents of the axilla. Superior aspect. The lung has
been removed.
Axillary
artery
The subclavian artery continues as the
axillary artery beyond the lateral edge of the first rib. Near the inlet, the
axillary artery lies posterior to the axillary vein (Figs 3.16 &
3.17) but more distally,
the artery lies lateral to the vein close to the humerus. The axillary artery
and parts of the brachial plexus that surround it are bound together by a fibrous
layer called the axillary sheath. Local anaesthetic injected inside the sheath
will spread to produce a brachial plexus nerve block. Coracobrachialis and the
short head of biceps brachii lie lateral to the artery, while pectoralis minor
crosses it anteriorly. By convention, the axillary artery is described in parts
which lie above, behind and below pectoralis minor. Distal to the lower border
of teres major, the vessel continues into the arm as the brachial artery (Fig.
3.18).
Branches of the axillary artery supply
the walls of the axilla and adjacent structures. The thoracoacromial artery
(Fig. 3.14) supplies the anterior wall, while the superior thoracic and lateral
thoracic arteries supply the medial and anterior walls. The thoracoacromial and lateral thoracic arteries also
supply part of the breast. The posterior wall is supplied by the subscapular
artery. The anterior and posterior circumflex humeral arteries (Fig.
3.18) pass laterally and
encircle the surgical neck of the humerus, supplying the shoulder joint and the
upper part of the arm. An important collateral circulation, the scapular
anastomosis is formed by communication between the circumflex scapular branch
of the subscapular artery and the suprascapular branch from the thyrocervical
trunk, a branch of the subclavian artery. These, and anastomoses involving
transverse cervical and posterior intercostal arteries, may enable blood to
bypass blockages in the subclavian and axillary arteries.
Axillary
vein
The venae comitantes of the brachial
artery unite with the basilic vein in the upper part of the arm and continue as
the axillary vein above the inferior border of teres major. The vein ascends
medial to the axillary artery (Fig. 3.16), passing behind pectoralis minor, and
crosses the lateral edge of the first rib to continue as the subclavian vein,
lying anterior to its companion artery. A major tributary of the axillary vein
is the cephalic vein, which ascends in the groove between deltoid and
pectoralis major. Just below the clavicle, it enters the axilla by piercing
the fascia above pectoralis minor (Fig. 3.14). The progress of a catheter
inserted proximally along the cephalic vein may be impeded by the acute
angulations often present near its termination in the axillary vein above
pectoralis minor. The axillary vein receives other tributaries, which in
general correspond to the branches of the axillary artery.
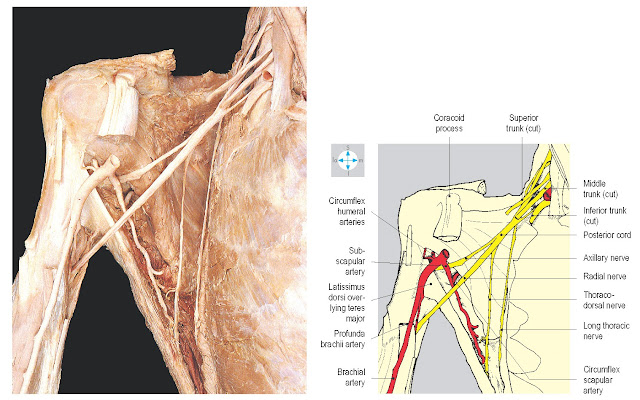 |
Fig.
3.18 Some
posterior branches of the brachial plexus seen after removal of the more
anterior parts of the plexus. Biceps brachii and coracobrachialis have been
excised.
Brachial plexus
The whole plexus is described here,
although only the divisions, cords and certain branches lie within the axilla.
The brachial plexus supplies the upper limb and consists of a branching network
of nerves derived from the anterior rami of the lower four cervical and the
first thoracic spinal nerves. Occasionally, the plexus receives a major
contribution from cervical nerve four (said to be a pre-fixed plexus) or from
the second thoracic nerve (post-fixed plexus). The plexus enables nerve fibres
originating in several spinal cord segments to be distributed to each
peripheral branch. Knowledge of the segmental arrangement and distribution is
necessary for accurate diagnosis in diseases or injuries involving the spinal
cord or the brachial plexus. The parts of the plexus are named, from proximal
to distal: roots, trunks, divisions and cords (Fig. 3.19). The five roots
(anterior rami) give rise to three trunks (superior, middle and inferior),
which emerge between scalenus medius and scalenus anterior to lie in the floor
of the posterior triangle of the neck (p. 326). The roots of the plexus lie deep
to the prevertebral fascia, while the trunks are covered by its lateral
extension, the axillary sheath. Each trunk divides into an anterior and a
posterior division behind the clavicle, at the apex of the axilla. Within the
axilla, the divisions combine to produce the three cords, which are named
lateral, medial and posterior, according to their relationships to the axillary
artery. Each cord ends near the lower border of pectoralis minor by dividing
into two terminal branches. Other branches of the plexus arise in the neck and
axilla directly from the roots, trunks and cords (Fig. 3.20). The anterior divisions form the lateral and
medial cords (Fig. 3.17), whose branches supply the flexor muscles of the arm,
forearm and hand, and the skin overlying the flexor compartments. The three
posterior divisions unite to form the posterior cord (Fig. 3.18), the branches
of which supply the extensor musculature of the shoulder, arm and forearm and
the skin of the posterior surface of the limb.
The axillary lymph nodes receive lymph
not only from the upper limb but also from the superficial tissues of the trunk
above the level of the umbilicus, including the breast.
The nodes are described in groups
according to their positions in the axilla. Anteriorly lies the pectoral group,
which drains the lateral and anterior aspects of the body wall including the breast.
Laterally, along the axillary vessels, is the humeral (lateral) group of nodes,
which receives most of the lymph from the upper limb. Posteriorly the
subscapular nodes receive lymph from the dorsal aspect of the body wall. Within
the axilla, efferent lymph channels drain centrally and then proximally to
apical nodes from which a subclavian lymph trunk arises; this terminates in the
root of the neck by joining, on the right, the right lymphatic duct or, on the
left, the thoracic duct. Sometimes the lymph trunks join the subclavian vein
directly (p. 330). Clinical examination often includes palpation of the axillary
lymph nodes, for example in breast disease. When malignant disease is present,
the axilla may be explored surgically to identify sentinel lymph nodes.
The principal vessels and nerves
entering or leaving the axilla are listed in Table 3.2.






