FRACTURE OF DISTAL
HUMERUS
In adults, fractures of the distal humerus often require surgical fixation
because they are usually caused by a high-energy injury and frequently are comminuted
and/or intra-articular in location. Fracture patterns include supracondylar,
transcondylar, intercondylar (T or Y), lateral or medial condyle, or epicondyle
and isolated capitellar or trochlear fractures. Intra-articular fractures may
be difficult to adequately assess on plain radiographs; therefore, CT scans may
be needed.
Surgical fixation can be with plates
and screws, or screws alone, depending on the particular fracture pattern.
Joint replacement has also become an option for distal humerus fractures that
may be too comminuted to be stabilized with plates and screws.
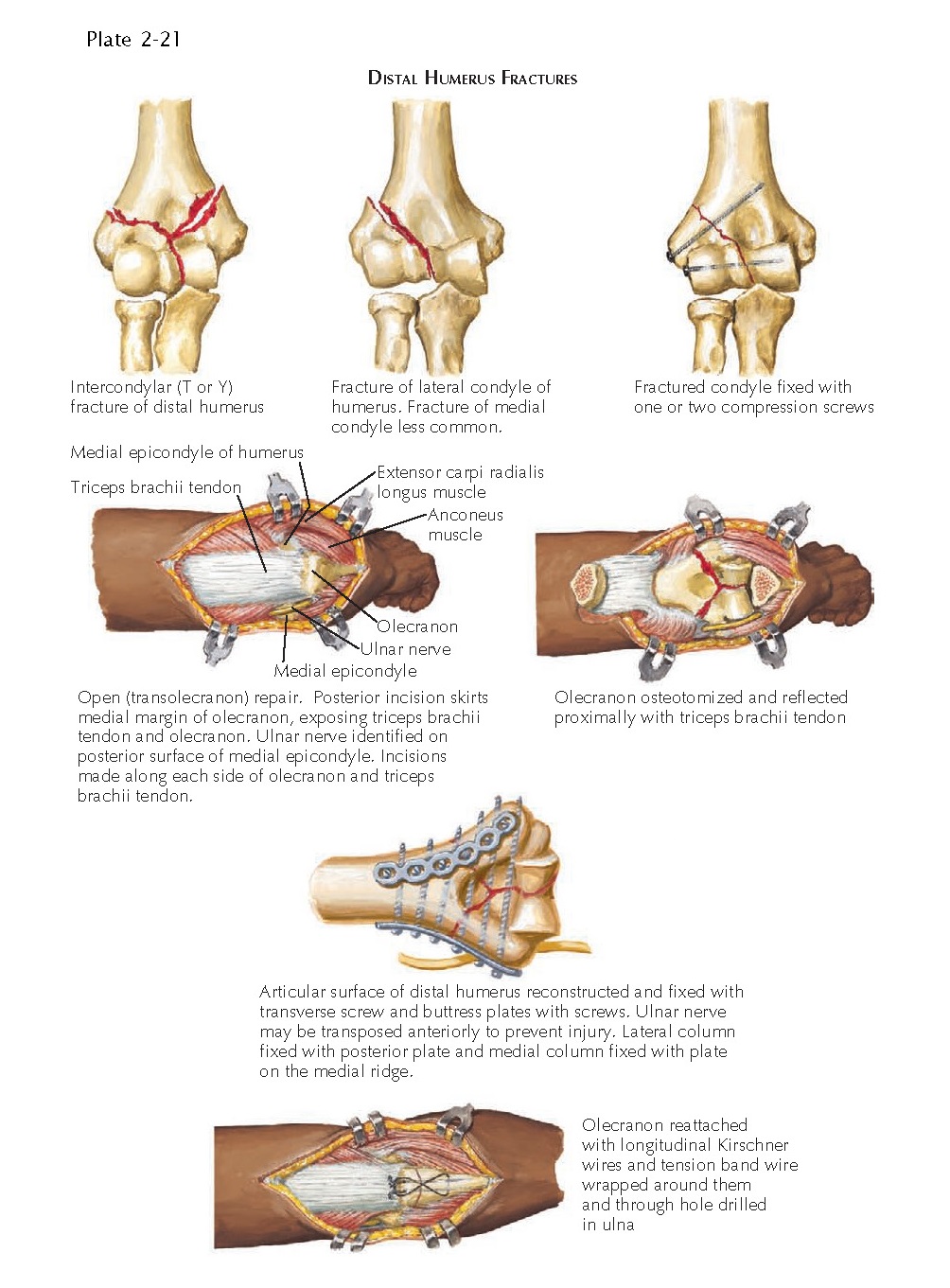
Complex Intra-articular
Fractures
Comminuted intra-articular fractures
of the distal humerus are among the more challenging orthopedic injuries, and
their reconstruction requires considerable surgical skill (see Plate
2-21). The major
complications include restricted elbow motion and early degenerative joint
disease.
Surgical fixation of comminuted
intra-articular fractures can be problematic: the distal fragments are small,
minimizing the number of available screw sites, and the fragments are primarily
cancellous bone, which compromises screw purchase. In addition, the surface of
the distal fracture fragments is primarily articular cartilage, which must be
protected, and the complex topography of this region can make reconstruction of
the normal anatomy difficult.
The structure of the distal humerus is
conceptualized as two bony columns diverging from the shaft. The medial column
includes the medial pillar of the distal humerus, the medial condyle and
epicondyle, and the trochlea. The lateral column includes the lateral pillar of
the distal humerus, the lateral epicondyle and condyle, and the capitellum. To
approach and fix intra-articular fractures of the distal humerus, an
intra-articular osteotomy of the olecranon is usually performed and the
olecranon and the aponeurosis of the triceps brachii muscle are reflected
proximally, exposing the entire distal humerus (see Plate 2-21). The ulnar nerve is also identified and
typically transposed as part of the surgical approach. Internal fixation of the
distal humerus first involves reconstructing the articular surface and holding
the fragments together with transverse Kirschner wires or lag screws. The
articular surface is then reattached to the shaft with plates and screws to provide stability in both
the anteroposterior and mediolateral planes. Current techniques utilize
bicondylar plating with precontoured plates that match the anatomy of the
distal humerus. Bicondylar plating can be performed with the plates at right
angles to one another (medial plate and posterolateral plate) or straight
across from one another (medial plate and lateral plate). The olecranon is
reattached with a precontoured plate to fit the olecranon or a tension band
wire (see Plate 2-21). Newer surgical approaches have been developed and are
now being utilized that avoid the need for an olecranon osteotomy while still
providing enough visualization of the distal humerus from appropriate fixation.
This can speed up recovery after surgery and avoids the risk of developing a
nonunion at the osteotomy site.
Total elbow arthroplasty has also
become an option for comminuted distal humerus fractures. In elderly patients
with poor bone quality, such fractures may be unable to be stably fixed with
plates and screws. Joint replacement allows early range of motion and function
for these otherwise devastating elbow injuries, without requiring bony healing
(see Plate 2-22). In younger patients with severely comminuted
distal humerus fractures that cannot be reconstructed with plates and screws,
elbow hemiarthroplasty is becoming a surgical alternative in select cases. This
replacement of only the humeral side of the elbow is a newer option in this
patient population that is typically considered too active for a complete elbow
replacement.
Early elbow range of motion is
important after plating or elbow arthroplasty to avoid stiffness. Protected
active and active-assisted exercises (flexion-extension, pronation-supination)
are encouraged soon after surgery to maintain range of motion in the elbow
joint.
Fractures of Lateral Condyle
Fractures of the lateral condyle can
involve the capitellum alone or extend medially to involve the lateral portion
of the trochlea (see Plate 2-21). Fractures of the lateral condyle are more
common than those of the medial condyle and are usually displaced and require
surgical fixation. As with any intra-articular fracture, open reduction and
internal fixation is performed to reestablish the articular surface as
accurately as possible and to allow early active motion. A plate and screws or
screws alone can be used for fixation, depending on the fracture pattern. In
fractures of the lateral condyle, both in adults and in children, it is
important to preserve all the soft tissue attachments, particularly
posterolaterally, to maintain the blood supply to the fragment. With rigid
internal fixation, the patient can begin active motion as soon as the soft
tissues have healed.
Fractures of Capitellum
Fractures of the capitellum alone are
uncommon and may be difficult to diagnose if the fracture fragment is very
small. Any effusion within the elbow joint together with displacement of the
fat pads on plain radiographs suggests either a capitellar fracture or other
nondisplaced fracture near the elbow.
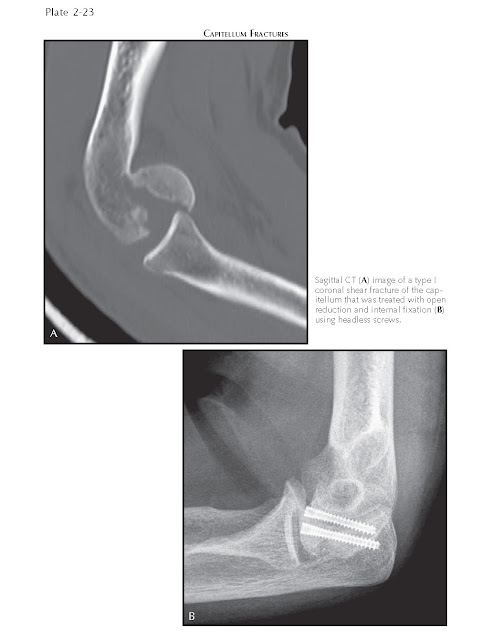
There are four types of capitellar
fractures. The type I (Hahn-Steinthal) fracture is a coronal fracture that
involves a large part of the osseous portion of the capitellum and is typically
treated with open reduction and internal fixation with one or two screws. This
method makes early joint motion possible in rehabilitation. These screws often
need to be placed on the articular surface in an anterior to posterior
direction and, therefore, are headless and countersunk (see Plate
2-23). The type II
(Kocher-Lorenz) fracture is a sleeve fracture that involves primarily the
articular cartilage with very little underlying bone. The fragment is often too
small to be fixed, and treatment includes excision of the fragment. Type II
fractures cause few subsequent problems in the elbow joint. Type III fractures
are comminuted and also may be difficult to fix, and a type IV fracture is
similar to a type I fracture, except that it extends more medially and includes
a major portion of the trochlea.
Fractures of Medial Epicondyle
The medial epicondyle is the common
origin of several flexor muscles of the hand and wrist. When the medial
epicondyle is fractured, the flexor muscles pull the fragment distally. The
injury is often accompanied by valgus instability of the elbow if the
collateral ligament is affected and by injury to the ulnar nerve. If there is
significant valgus instability of the elbow, the epicondyle must be reduced to
its anatomic position and secured with a pin or a screw. During the surgical
procedure, care must be taken to protect the ulnar nerve from inju y, and ulnar
nerve transposition may be necessary.