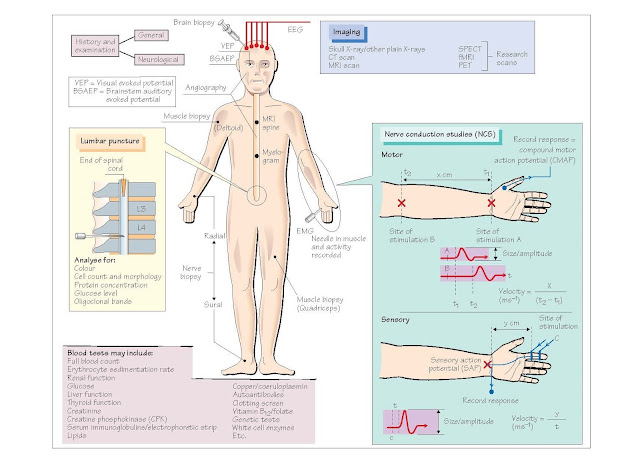
Investigation Of The Nervous System
The key to investigating
any patient is through their history and examination, as this will highlight
the likely nature and site of the problem.
At the end of the history
and examination one should have formulated a hypothesis of where the problem
lies and what the problem could be, which will then guide investigations.
Blood tests
A large number of tests
are available (see figure for examples).
Imaging (see also Chapter 53)
· Plain X-rays are rarely of value in
the diagnosis of neurological disease, unless one suspects the patient has a
related disease in another site such as the chest (e.g. lung cancer).
· Computed tomography (CT) gives
detailed X-ray images of the brain, skull and lower spine. It is useful for
diagnosing structural lesions such as tumours, major strokes or skull
fractures. It is widely available but has limited resolution especially in the
posterior fossa and cervicothoracic spinal cord.
· Magnetic resonance imaging (MRI) is
a noisy, claustrophobic procedure which relies on patient cooperation. It
provides detailed images of all parts of the brain and spinal cord and the use
of different sequences has increased its utility and diagnostic strength. It
does not involve any radiation.
· Magnetic resonance angiography and
venography (MRA/MRV) scans delineate the major blood vessels to, within and
from the brain. They are primarily used to look for significant narrowing
(stenosis) of the extracranial carotid arteries in the neck, aneurysms in the
brain and blockage of the major venous sinuses in the brain, but are not as sensitive as
angiography.
· Angiography involves the passing of
a small catheter to the origin of the major blood vessels of the brain
(both carotid and vertebral arteries), and a small amount of dye is injected.
The dye can then be followed using a video and images captured rapidly over
time as the dye passes through the vascular tree. The proce- dure is invasive
and carries a small risk of complication, but is useful in accurately
delineating any vascular abnormalities (e.g. carotid stenoses, aneurysms,
arteriovenous malformations and venous sinus thrombosis). It can also be used
to look for specific vascular abnormalities in the spinal cord.
· Myelography is rarely used nowadays
to delineate abnormalities in the spinal cord because of the non-invasiveness
and resolution of MRI. However, it can be helpful in some circumstances and
involves injecting a radio-opaque dye via a lumbar puncture into the subarachnoid
space around the spine.
· Single photon emission computed
tomography (SPECT) involves radioactive isotopes which typically provide
information on per- fusion within the brain. It has low resolution.
· Positron emission tomography (PET)
detects the release of positrons from specific substances that bind to certain
chemical sites within the brain. It is only used to localize small occult
tumours in patients with suspected paraneoplastic syndromes at the moment.
Electrical tests
· Electrocardiography (ECG) is an
electrical recording from the heart, and is performed in many patients with
neurological disease, especially those with muscle disease, blackouts or some
genetic disorders (e.g. myotonic dystrophy).
· Electroencephalography (EEG)
measures the electrical activity and rhythms of the brain and is helpful in
patients with decreased levels of consciousness, epilepsy (see Chapter 61) and
some patients with sleep disorders (e.g. narcolepsy; see Chapter 43).
· Nerve conduction studies (NCS)
involve stimulating both sensory and motor nerves and measuring the response.
The general principle is that one stimulates at one site of the nerve and
records at another site or the muscle it innervates. The size and speed of the
response are important. Loss of myelin (demyelination) slows the speed of
conduction, while a loss of axons gives a smaller response but normal
conduction velocity. It is useful in determining whether the patient has a neuropathy,
what type (demyelinating versus axonal) and the extent (focal or generalized).
· Electromyography (EMG) involves
placing a needle into the muscle and recording the electrical activity within
it. It is useful in the diagnosis of muscle disease and in patients with motor
neuronal loss as occurs in motor neurone disease (MND)
because EMG can show the extent of denervation, helping in the diagnosis.
· Evoked potentials (EPs) can be
recorded from the visual pathway (visual-evoked potential or responses; VEP),
auditory pathway (brainstem auditory-evoked potential BSAEP) or peripheral
nerves in the arms or legs (somatosensory-evoked potential). The test involves
stimulating the peripheral receptor (eye, ear or median/posterior tibial nerve) and
measuring the cortical response.
This gives a measure of
conduction that has both a peripheral and CNS component. The most commonly used
test is VEP in multiple sclerosis to look for asymptomatic
demyelination in visual pathways.
• Central
motor conduction time (CMCT) measures the time from stimulating the motor
cortex to measuring a muscle response in the periphery such as the hand. It is
not routinely available and can be used as a measure of integrity of the
descending corticospinal tract assuming that there is no dysfunction within the
peripheral motor apparatus.
• Thermal
thresholds are a subjective test designed to look at small fibre responses in
patients. It relies on the patient detecting changes in temperature in the
hands and feet. It is not routinely available.
Cerebrospinal fluid
analysis
Cerebrospinal fluid
(CSF) can be obtained from a number of sites but is routinely obtained by a
lumbar puncture, which involves passing a small needle into the subarachnoid
space in the lower lumbar spine. CSF should be clear and sent for analysis to
include the following:
• Numbers
of certain cell types are typically raised in infections (e.g. meningitis and
encephalitis) as well as in malignant meningitis (where cancer
cells seed themselves along the meninges).
• Culture
of the CSF to look for infective organisms, including Gram staining in
meningitis and polymerase chain reaction (PCR) for the causative organism in
some infections of the CNS (e.g. herpes simplex virus in herpes encephalitis).
• Glucose
levels, which can be low in certain types of infection or meningitis and
metastatic tumours growing in the meninges.
• Protein
levels, which can be raised in some types of neuropathy, tumour and in lesions
blocking spinal CSF flow.
• Oligoclonal
bands indicative of immunoglobulin synthesis specifically within the CNS,
typically seen in multiple sclerosis.
Nerve/muscle biopsy
In cases where there is
evidence of nerve or muscle disease, a biopsy may be helpful in identifying the
defect more specifically. Typical biopsy sites are the radial and sural nerves
and the quadriceps and deltoid muscles.
Brain biopsy
This is routinely
performed in patients with brain tumours to confirm the diagnosis and to some
extent predict prognosis. In some cases of progressive neurological disease for
which no obvious cause can be found, a biopsy looking specifically for
inflammation in the blood vessels (vasculitis) as well as prion disease may
be considered.