Neurochemical Disorders II: Schizophrenia
Schizophrenia is a syndrome characterized by
specific psychological manifestations, including auditory hallucinations,
delusions, thought disorders and behavioural disturbances. It is a common
disorder with a lifetime prevalence of 1% and an incidence of 2–4 new cases per
year per 10 000 population. It is more common in men and typically presents
early in life. Like all psychiatric disorders there is no diagnostic test for
this condition, which is defined by the existence of key symptoms.
· Positive symptoms:
•
delusions:
abnormal or irrational beliefs, held with great conviction and out of keeping
with an individual’s sociocultural background;
•
hallucinations:
perceptions in the absence of stimuli.
· Negative symptoms:
•
blunting
of mood, apparent apathy, lack of spontaneous speech and action;
•
disordered
speech.
Aetiology
A distinction used to be
made between type 1 and 2 schizophrenia but this has fallen out of fashion as
it may relate more to the length of time that the individual has had the
condition. The cause of schizophrenia is unknown but a number of aetiological
factors have been suggested:
• Genetic
factors: first-degree relatives of people with schizophrenia have a greatly
increased risk of developing the disease; around 10% for siblings, 6% for parents
and 13% for children. Concordance rates in twins are relatively high with
figures varying from 42% to 50% for monozygotic twins and between 0 and 14% for
dizygotic twins. Recent Genome Wide Association Studies (GWAS) have also
confirmed a genetic basis for the condition.
• Environmental
factors: e.g. infections during pregnancy also may have a role, with adoption studies
demonstrating the importance of both genetic and environmental factors. In
these studies gene–environment interactions have been demonstrated in children
of schizophrenic parents adopted into good versus disturbed adoptive
families. In this latter respect one influential theory relating to a family
cause appeals to high levels of ‘expressed emotion’ (hostility, lack of
emotional warmth, over-involvement) as a risk for relapse.
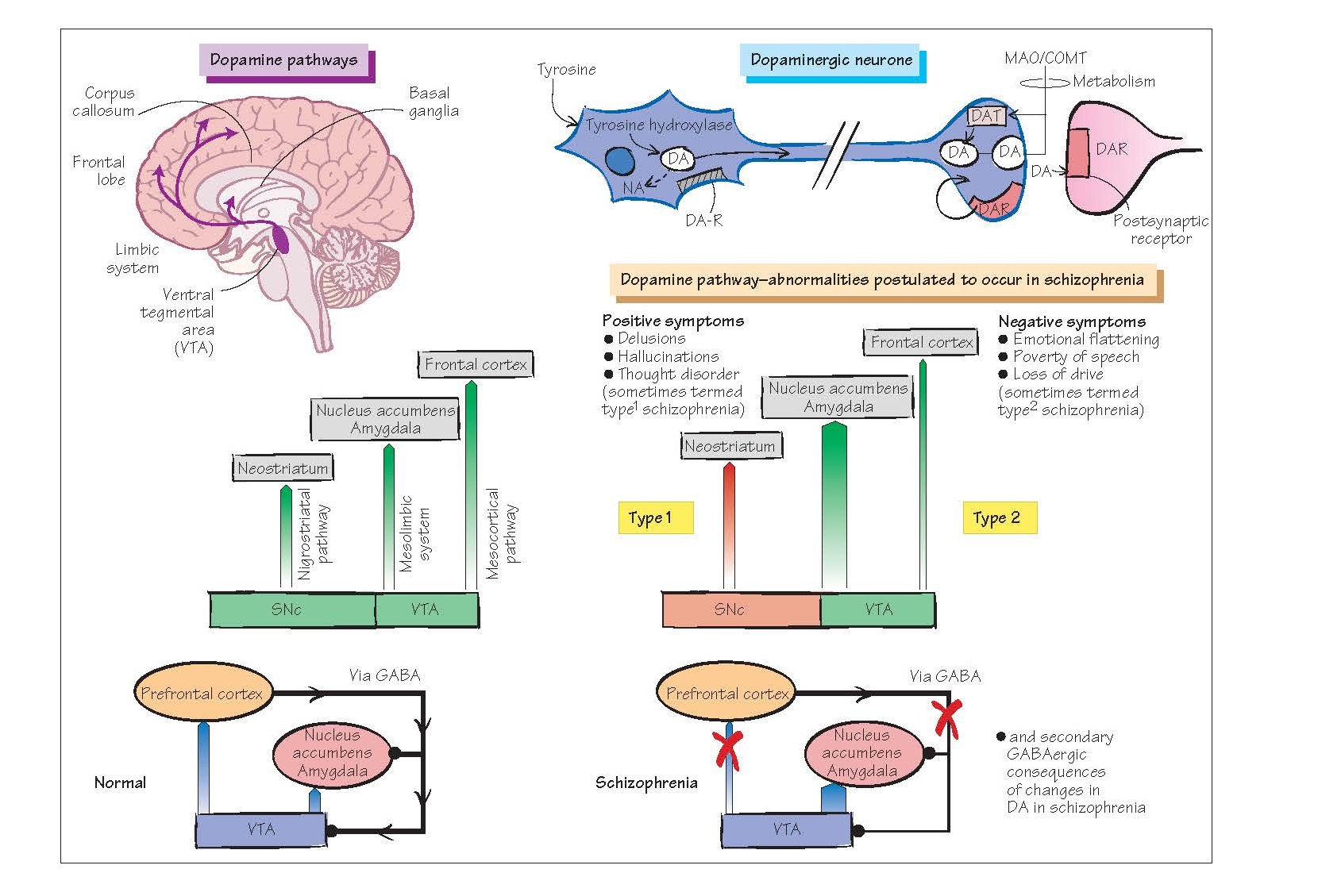
The dopamine
hypothesis of schizophrenia
Basic model
Simply stated, this
embodies the idea that schizophrenia is caused by up-regulation of activity in
the mesolimbic dopamine system. The evidence for this theory comes from:
· Dopamine-blocking drugs show an
antipsychotic effect.
· Drugs that up-regulate dopamine can
produce positive symptoms of psychosis (e.g. amphetamines).
· Some neuroimaging studies in
patients have found evidence of dopamine up-regulation.
The dopamine hypothesis
has been criticized for the lack of direct evidence in its favour and for
certain inconsistencies:
· Dopamine agonists do not produce all
of the symptoms of schizophrenia (notably, they do not produce negative
symptoms);
· Dopamine-blocking drugs do not act
immediately – there may be a long period before symptoms begin to resolve.
Revised model
The above
inconsistencies led to the revision that both dopamine up-regulation and
down-regulation must be invoked to account for the core features of schizophrenia,
with the positive symptoms arising from up-regulation of mesolimbic dopamine
function and the negative symptoms from down-regulation of mesocortical
function.
However, many still
think this as an inadequate explanation of such a complex disorder, and there
is a view that schizophrenia is associated with N-methyl-D-aspartate (NMDA)
(glutamate) receptor hypofunction. This arose from observations
that NMDA blockers such as phencyclidine (‘Angel Dust’) and ketamine (widely
used in anaesthesia) produce a psychotic state (including negative symptoms)
that is held to be more strongly redolent of schizophrenia than the psychosis
produced by dopaminergic agents. There- fore, it has been proposed that
glutamate hypofunction may account for both up-regulation of the mesolimbic
dopamine system, from a diminished excitatory drive of GABAergic inhibition
(i.e. an attenuation of the ‘brake’ system), and down-regulation of the
mesocortical system because of diminished direct drive (the ‘activating’
system).
Cognition in
schizophrenia
Whilst schizophrenia is
traditionally described in terms of psychotic symptoms, there is increasing
evidence of cognitive deficits, particularly in the memory domain,
that may accompany (and perhaps precede) the onset of these symptoms.
Treatment
The mainstay of therapy
in schizophrenia remains the use of drugs that block dopamine receptors, of
which there are at least five subtypes in the brain (D1–D5 receptors; see
Chapter 19). These agents (e.g. chlorpromazine) are called antipsychotics or
neuroleptics. Most neuroleptics block D1 receptors but there is a close
correlation between the clinical dose of antipsychotic drugs and their affinity
for D2 receptors, suggesting that blockade of this receptor subtype may be
particularly important. D2 receptors are found in the limbic system and in the
basal ganglia, and D3 and D4 receptors are found mainly in the limbic areas.
Antipsychotic drugs (eg
chlorpromazine, haloperidol) require several weeks to control the symptoms of
schizophrenia and most patients require maintenance treatment for many years.
Relapses are common even in drug-maintained patients. Unfortunately,
neuroleptics also block dopamine D2 receptors in the basal ganglia, often
producing distressing and disabling movement dis- orders (e.g. parkinsonism,
acute dystonic reactions, akathisia [motor restlessness] and tardive dyskinesia
[orofacial and trunk movements]) which may be irreversible; see Chapter 42).
Blockade of D2 receptors in the pituitary gland causes an increase in prolactin
release and endocrine effects (e.g. gynaecomastia, galactorrhoea; see Chapter
11). Many neuroleptics also block muscarinic receptors (causing dry mouth,
blurred vision, constipation), α-adrenoceptors (postural hypotension) and
histamine H1 receptors (sedation).
Atypical drugs
Some newer drugs have a
reduced tendency to cause movement disorders and are referred to as atypical
agents (e.g. clozapine, risperidone, olanzapine, quetiapine).
With the possible exception of clozapine, these drugs are not more efficacious
than the older antipsychotic drugs. Clozapine is restricted to patients
resistant to other drugs because it causes neutropenia or agranulocytosis in
about 4% of patients. Risperidone and other newer atypical agents are increasingly
used in the treatment of schizophrenia because they are more acceptable to
patients.
It is not clear why some
neuroleptics are ‘atypical’. Clozapine may be atypical because in addition to
being a dopamine D2 antagonist it is a potent blocker of 5-HT2
receptors.