Shoulder And Elbow
Injuries
The extreme mobility of the shoulder joint, which
relies on soft tissues – muscles, ligaments and cartilage – for stability,
comes at a price. The shoulder is relatively unstable, and prone to stiffness
if not used. There is a wide range of injury patterns, which change according
to the age of the patient.
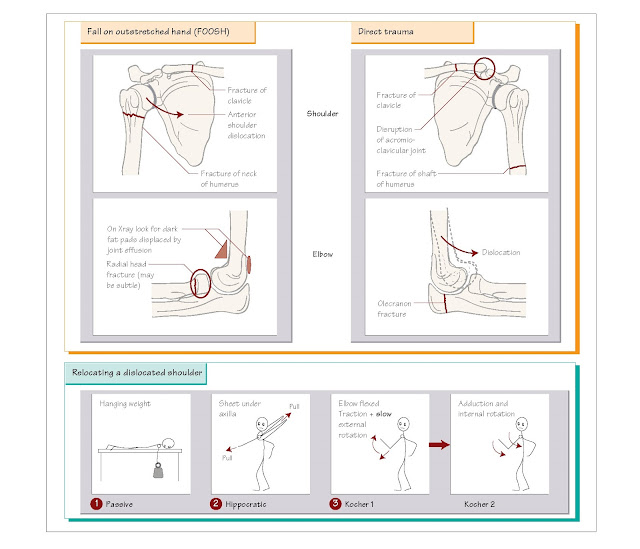
History
In any
injury affecting the upper limb, dominance (handedness) and occupation and
hobbies must be recorded. Shoulder pain can also be referred, e.g. cardiac,
diaphragmatic, respiratory. Injury is usually caused by either a fall onto
outstretched hand (FOOSH) or direct trauma.
Examination
Look Compare with the other
side.
Feel Start at the medial end
of the clavicle and work laterally, feeling for tenderness of clavicle,
coracoid process, acromioclavicular (AC) joint, humeral head and greater
tuberosity. Feel the olecranon, epicondyles and radial head. An elbow effusion
may be felt below the radial head.
Move Limited or painful
shoulder movement warrants an X-ray; very little movement will be possible with
a dislocated shoulder or fracture. A full range of elbow extension makes
fracture unlikely.
Neurovascular examination
Specific
injuries and their corresponding neurovascular deficits are:
• Shoulder dislocation and fracture neck of humerus: test the axillary
nerve – loss of sensation over lower deltoid area.
•
Humeral shaft fractures – radial nerve.
•
Medial epicondyle fracture – ulna nerve injury.
•
Elbow dislocations – brachial artery and median nerve.
Imaging
Plain X-rays
are indicated in most patients presenting with shoulder pain and reduced range
of movement after trauma. Elbow fractures are very unlikely if there is full
elbow extension. Fractures are difficult to see and radiographs should be
examined carefully for evidence of an effusion: the dark shadows caused by the
anterior and posterior fat pads.
Management
Analgesia is
achieved by immobilisation (e.g. sling), and oral analgesics before imaging.
Patients with severe pain and deformity require intravenous opiates and early
assessment. Early active move- ment of the shoulder is important to avoid
stiffness in the elderly.
Ensure
urgent orthopaedic referral for:
•
Any fracture with neurovascular compromise.
•
Open fractures, which require urgent antibiotics.
Common diagnoses
Fractured clavicle
This injury
most commonly occurs at the junction between the middle and outer third. Most
heal with good function by providing rest in a sling and analgesia.
Acromio-clavicular joint injuries
Acromio-clavicular
joint (ACJ) injuries are caused by fall onto tip of shoulder, causing
disruption to the ACJ and ligaments. With complete disruption, the clavicle
will ‘float’ above the acromion. ACJ injuries are treated with analgesia, rest
in a sling and physiotherapy in the first instance, but the more severe grades
of disruption may need fixation later.
Dislocated shoulder
The shoulder
usually dislocates anteriorly (95%) from a fall with the arm in the ‘hailing a
taxi’ position – the humerus is externally rotated and abducted. The humeral
head may be palpable and the patient will support the arm, holding it by their
side.
There are
many different reduction techniques, each with their own proponents. It is
generally best to start with a passive technique that requires only nitrous
oxide/oxygen analgesia and can be conducted by nursing staff. The active
techniques require intravenous analgesia ±
sedation (Chapter 6).
• Passive:
hanging weight technique. The patient lies prone on a couch with the arm
hanging down with a 2–5 kg weight suspended from their wrist.
• Active:
Hippocratic technique. Traction of the patient’s arm, together with mild rotation. The
traditional method of counter-traction involved the doctor’s ‘stockinged foot’
in the patient’s axilla. The modern version uses a sheet under the axilla so an
assistant at the head of the bed can provide counter-traction.
• Active:
modified Kocher’s technique. This technique must not be rushed and requires good
analgesia and sedation.
1. Flex elbow, continuous
gentle traction.
2. Using the forearm as a
lever, the humerus is externally rotated to almost 90° very slowly to
overcome pectoral spasm.
3. The arm is brought
across the body and the humerus internally rotated to achieve reduction.
Reduction
should be confirmed on X-ray, which may show any damage to the humeral head.
Patients with a first dislocated shoulder should have the shoulder immobilised
for 6 weeks to allow the capsule to heal. Patients with multiple dislocations
need surgery to stabilise the shoulder.
Fractured neck of humerus
This injury
is common in the elderly, due to FOOSH; underlying causes for falls should be
sought (Chapter 30). Early mobilisation with appropriate analgesia is necessary
to avoid long-term stiffness (‘frozen shoulder’) that may be far more disabling
than the original injury. Displaced fractures may require reduction ± fixation.
Dislocated elbow
Hyperextension
of the elbow forces the humerus anteriorly over the coronoid process of the
ulna. Neurovascular status should be checked, and this should be reduced by
traction under sedation.
Fractured head of radius
This is the
most common elbow fracture, which can be difficult to see on plain X-ray,
although the elbow effusion ‘fat pad sign’ will be visible. Diagnosis can be
confirmed by tenderness over the radial head, and reduced pronation/supination.
Most fractures make a good recovery with analgesia and early mobilisation.
Fractured shaft of humerus
Twisting
injuries produce spiral fractures, bending injuries transverse fractures.
Radial nerve injury can occur in fractures of the middle third of the humerus.
Diagnoses not to miss
Posterior dislocation of shoulder
This injury
is most common after epileptic fits or electrical injury forcing contraction of
the strong latissimus dorsi muscles. Posterior dislocation is difficult to spot
on X-ray: there is reduced glenohumeral overlap and the greater tuberosity is
not visible, creating the ‘lightbulb sign’: the humeral head appears
symmetrical. If in doubt, ask for an axillary view X-ray.
Scapular fracture
Scapular
fractures can be difficult to see on X-ray, but are usually very painful due to
distension of the tight capsule and may need admission for analgesia.
Significant energy is necessary to fracture a scapula, and other injuries
should be sought.