CYSTITIS
Urinary tract infections (UTIs) can involve the
bladder alone (lower UTI, also known as acute cystitis) or extend to the renal
pelvis and parenchyma (upper UTI, also known as acute pyelonephritis). If
untreated, such infections can progress in vulnerable hosts to systemic
bacterial disease, known as urosepsis.
Although “cystitis” refers, in the strictest sense, to
inflammation of the bladder, by far the most common cause is bacterial
infection, which occurs when bacteria ascend to the bladder from the urethra.
Thus use of the term “cystitis” without additional qualification usually implies
bacterial infection of the bladder. In contrast, “nonbacterial cystitis” is
often used to specify bladder inflammation associated with viruses, parasites,
radiation, chemical irritants, and other agents.
Cystitis is considered “uncomplicated” when it occurs
in women with anatomically and neurologically normal urinary tracts. In
contrast, cystitis is considered “complicated” when it occurs in the setting of
structural or functional abnormalities of the urinary tract; in association
with an indwelling urinary catheter; in conjunction with an upper urinary tract
infection; or in men, pregnant women, or hospitalized patients.
PATHOPHYSIOLOGY
Acute uncomplicated cystitis occurs in women when
enteric flora from the perianal region colonize the adjacent vaginal introitus
and then ascend the urethra to reach the bladder. Escherichia coli (E.
coli) is the most common pathogen, accounting for nearly 80% of all infections.
Other common pathogens include Staphylococcus saprophyticus, Klebsiella
pneumoniae, and Proteus mirabilis, in order of descending frequency.
Less commonly, Citrobacter and Enterococcus may be responsible.
Complicated cystitis, in contrast, often involves additional pathogenetic
mechanisms, such as the presence of a urinary catheter or bladder outlet
obstruction, and in these cases the responsible pathogens differ. E. coli,
for example, accounts for only 35% of such infections. Instead, there is a
higher prevalence of other gram-negative species, such as Pseudomonas
aeruginosa, and gram-positive organisms, such as Enterococcus and coagulase negative staphylococci.
In any patient, the likelihood of urinary tract
infection depends on the balance between host defenses and pathogen virulence factors. In the host, several
mechanisms defend the urinary tract from infection. For example, the low pH and
high urea concentration in urine inhibit bacterial proliferation. In addition,
the presence of certain molecules on the epithelial surface of the urinary
tract such as human
defensins, Tamm Horsfall
proteins, and glycosaminoglycans confer protection against bacterial adhesion. Lastly, the flow of urine
itself plays an important mechanical role in the clearance of bacteria.
These protective mechanisms, however, may be over come or impaired in certain circumstances. For
example, when women engage in sexual intercourse, there is often substantial
displacement of both fecal and vaginal flora toward the urethra. This risk
further increases with the use of diaphragms or spermicides, which may render
the vaginal environment more hospitable to the proliferation of uropathogens.
In older women, a decline in estrogen can lead to a loss of the protective
lactobacilli that are part of the normal vaginal flora, enabling increased colonization with uropathogens. Pregnancy alters the
pH and osmolality of urine, making it more favorable to bacterial growth.
Several pathologic conditions can also interfere with
normal host defenses and increase the likelihood of infection. Diabetes
mellitus, for example, has several pathologic effects that predispose affected
individuals to infection. Urinary stasis, which can result from anatomic or
functional obstruction, makes it more difficult to clear bacteria from the
bladder. Indwelling urinary catheters also increase the infection risk by
facilitating migration of uropathogens into the bladder. Bacteria adhere to the
catheter surface and contribute to the creation of a biofilm, which contains
bacteria, bacterial glycocalyces, host proteins, and urinary salts such as
apatite and struvite. The bacteria can then travel along the catheter beneath
this biofilm until they reach the bladder. Indeed, long-term use of urinary
catheters will always result in colonization and infection. In contrast,
urinary catheters that are used for fewer than 7 days are less likely to cause
clinically significant infections as long as the catheter connections are left
undisturbed and a closed drainage system is scrupulously maintained.
Uropathogenic organisms also have several factors that
determine their invasiveness, persistence, and site of infection. Genetic
differences both within and across species can modulate adhesion to host cells
and resistance to the defenses described above. For example, some serogroups of
E. coli have surface fimbriae that offer improved adhesion and facilitate
extension to the upper urinary tract. Similarly, bacteria that express K capsular
antigens, such as Klebsiella species, are resistant to neutrophil
phagocytosis. Finally, motility mechanisms, such as flagellation, permit certain
bacteria to navigate the urinary tract against the flow of micturition.
PRESENTATION AND DIAGNOSIS
The major symptoms of cystitis include painful and
frequent urination, urgency, hesitancy, and pelvic pressure. These symptoms reflect irritation of urethral and vesicular mucosa. Foul
smelling, discolored, or blood tinged urine may also be noted. The presence of fever or abdominal pain
should prompt suspicion for upper tract disease (see Plate 5-5).
In certain populations, such as the elderly, symptoms
may be less specific and include depressed mental status and failure to thrive,
or there may be no symptoms at all. Children less than 2-years-old may also
have non-localizing symptoms. These differences likely reflect an inability to
mount an efficient immune response.
Because urethritis can sometimes mimic the symptoms of
cystitis, patients should be evaluated for possible gonorrhea or Chlamydia urethritis,
as well as for bacterial
vaginitis or genital herpes. In addition, the differential must include the
numerous causes of non bacterial cystitis. For example, trauma may cause bladder inflammation
and is often seen in women after forceful sexual intercourse. Interstitial
cystitis (also known as bladder pain syndrome) may also be associated with
cystitis-like symptoms. Hemorrhagic cystitis is most commonly seen in patients
undergoing cyclophosphamide treatment but can also result from adenovirus infection, especially in children. Finally, radiation therapy
can cause cystitis secondary to scarring.
After a careful history is taken to assess for the
above diagnoses, a midstream urine sample should be collected in a sterile
fashion and sent for urinalysis with microscopic evaluation. On urine dipstick,
a positive leukocyte esterase indicates the presence of white blood cells,
whereas positive urine nitrites reflect the presence of bacteria, which reduce
urinary nitrates. In the setting of suggestive symptoms, these dipstick results
may be enough to warrant empiric antibiotic treatment for cystitis in otherwise
healthy young women.
On microscopy, the presence of clinically significant
pyuria, defined as more than 10 leukocytes per cubic millimeter, suggests active
infection and should prompt empiric therapy in a patient with suggestive
symptoms. Microscopic evaluation can detect bacteria in the urine but is not
diagnostic, as false positives can occur due to unsterile collection technique.
A urine culture should be performed to confirm the
diagnosis, identify the pathogen, and determine its antibiotic susceptibilities.
Infection is probable if culture yields more than 105 colony forming units
(CFUs) per milliliter (mL) of a voided sample, or 104 CFUs/mL of a collected
sample (i.e., with a catheter). Some women may have symptoms of cystitis and
pyuria, but with either low bacterial titers or no growth on cultures.
Urethritis from other causes should be considered in these cases, such as
infection with Chlamydia trachomatis or Neisseria gonorrhoeae.
Imaging is generally not required in patients with
acute uncomplicated cystitis, but ultrasonography or computed tomography may be
pursued in those sus pected of having complicated disease or anatomic abnormalities.
TREATMENT
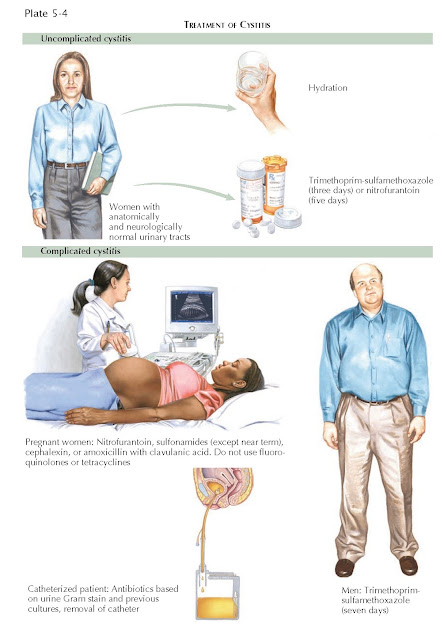
In cases of uncomplicated cystitis, the Infectious
Diseases Society of America recommends empiric treatment with
trimethoprim-sulfamethoxazole (TMP-SMX). A 3-day course is often adequate. A
5-day course of nitrofurantoin is another acceptable first-line treatment. In
certain areas of the United States, where there is concern for resistant E.
coli, a fluoroquinolone may be considered as the initial agent of choice.
Among fluoroquinolones, ciprofloxacin has been shown to have the highest efficacy in short courses. Other drugs that may be used include cephalosporins, amoxicillin with
clavulanic acid, and tetracyclines. If the patient has a history of prior
infections, susceptibilities on prior cultures should be examined before
choosing the initial treatment.
When initiating treatment, rapid hydration of the
patient can increase urine production and facilitate clearance of some bacteria
through voiding. As discussed earlier, urinary pH plays an integral role in
the innate antibacterial
activity of urine. Ingestion of cranberry juice (in large quantities) can
acidify the urine because cranberries contain precursors of hippuric acid, a
weak organic acid. Hence, urine becomes a less hospitable medium for bacterial
overgrowth, helping prevent both extension of current infection and future
bacterial overgrowth.
In complicated infections, the duration and choice of therapy depend on the population in question.
For pregnant women,
nitrofurantoin, sulfonamides, cephalexin, and amoxicillin with clavulanic acid
should be considered, although sulfonamides should not be used near term.
Fluoroquinolones and tetracyclines are classified as class C drugs for pregnant
women because of their teratogenic effects. The duration of treatment for a
lower UTI in a pregnant woman ranges from 3 to 7 days, with shorter courses
favored to minimize antibiotic exposure.
In young ambulatory men, the presence of UTI should
raise suspicion for anatomic anomalies and may prompt further evaluation with
imaging studies. In older men, UTIs may occur in the setting of prostatic
disease or catheterization. The choice of antibiotics for men is similar to
women, but the duration of therapy should be extended to 7 to 10 days.
For chronically catheterized patients or residents of
long-term facilities, the choice of an initial antibiotic agent should be based
on local patterns of resistance, including susceptibility data from prior
infections. Initial agents may include β-lactams or later generation
cephalosporins, such as ceftriaxone or cefepime. If a UTI occurs in the
presence of a urinary catheter, the catheter must be removed or changed.
Antibiotic therapy should be adjusted after cultures
reveal sensitivities. In high-risk populations, including pregnant women and
children, a repeat urinalysis and urine culture should be performed 2 weeks
after the completion of the antibiotic course to document clearance of the
infection. Low-grade bacteriuria may persist after treatment and may represent
colonization in a patient who has otherwise shown clinical improvement (see
Plate 5-7).
PROGNOSIS
The prognosis of cystitis is usually excellent, but
recurrent UTIs are common. Women who experience a UTI have at least a 20%
probability of developing another one within 6 months.
UTI recurrence may be attributable to either relapse
or reinfection. A relapse occurs 1 to 2 weeks after completion of treatment and
involves the same pathogen responsible for the initial disease. Relapse
indicates inadequate treatment, undiagnosed upper tract infection, or
obstructive disease such as renal calculi or, in men, prostatic enlargement.
Patients may need up to 2 weeks of antibiotics. Those with a second symptomatic
relapse warrant a repeat course of antibiotics for 2 to 6 weeks, depending on
the pathogen and its susceptibilities. Patients with relapsing disease should
be evaluated for possible predisposing factors.
A reinfection can also occur shortly after initial
therapy. Unlike in relapse, however, the causative organism may be different in the second episode.
Reinfection is especially common in cases where there
are ongoing niduses of infection, such as urinary catheters with established
biofilms. The management strategies are the same as those outlined above for
first-time episodes. The source of infection should be identified and eliminated
if possible.
Some patients will require prophylactic treatment to
prevent recurrent infection. Some young women, for example, experience frequent
UTIs associated with sexual intercourse. These patients should be advised to void after
sexual activity and can be prescribed antibiotics for single-dose postcoital
chemoprophylaxis. Trimethoprim-sulfamethoxazole, nitrofurantoin, or
ciprofloxacin can be used in this setting. In postmenopausal women, use of
intravaginal estriol cream has been shown to decrease the recurrence of UTIs.
Other nonspecific therapies, such as hydration and maintenance of an acidic
urine pH, are also reasonable options.