POLYARTERITIS NODOSA
Polyarteritis nodosa is a rare chronic form of vasculitis of the medium to small vessels with significant cutaneous and systemic manifestations. It is a rare condition, with an estimated incidence of 5 per 1,000,000 persons. The symptoms depend on the organ system involved and the extent of vasculitis. Uniquely and for unknown reasons, the respiratory system is spared. Polyarteritis nodosa has been found in some cases to be a chronic, non life-threatening disease that affects only the skin. More often, it is a multisystem disease, with the skin being affected along with other organ systems. Many other organ system may be involved, and the skin features may be the presenting sign of the disease. Excisional skin biopsies of cutaneous lesions of polyarteritis nodosa show the characteristic necrotizing vasculitis of medium vessels within the deep reticular dermis. The cutaneous diagnosis of polyarteritis nodosa should alert the clinician to the possibility of systemic disease, and appropriate testing should be undertaken to evaluate for widespread disease. Most cases of polyarteritis nodosa are idiopathic, but this condition can be seen in association with viral infections, malignancy, or autoimmune disease. Coinfection with the hepatitis B virus is the most classic and most frequent association with polyarteritis nodosa.
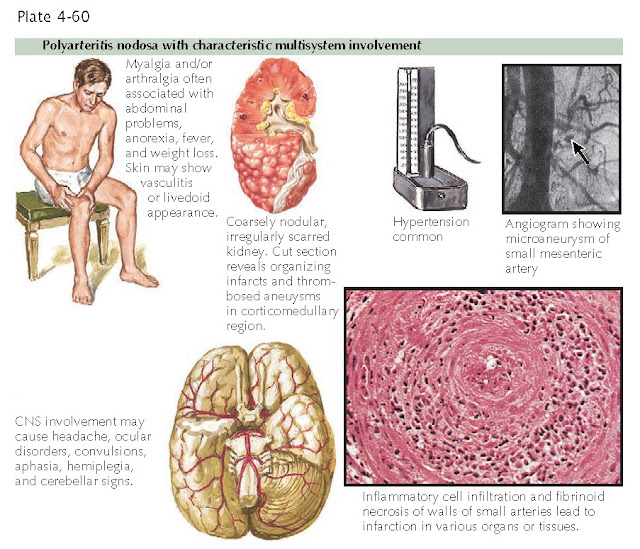
Polyarteritis nodosa with characteristic multisystem involvement
Clinical Findings: The primary cutaneous manifestation of polyarteritis nodosa is palpable
purpura. The cutaneous findings tend to be spread over wide areas of the body
and are not found entirely in dependent regions, as is the case with
leukocytoclastic vasculitis. Deeper, tender dermal nodules may form. These
nodules usually follow the course of an underlying artery. The patient may
develop livedo reticularis of the extremities, and secondary ulcerations may
form as the vasculitis progresses and causes necrosis of the overlying skin.
The diagnosis of the type of vasculitis is difficult to make from clinical
examination alone. Tissue sampling is needed to determine the type of vessel
affected by the inflammatory vasculitis. Polyarteritis nodosa has also been
shown to have nonspecific findings, such as red macules and papules, that mimic
drug eruptions or viral infections. If the only organ system involved is the
integumentary system, the prognosis is good, and the disease typically follows
a chronic, treatable course.
Once the diagnosis of cutaneous polyarteritis nodosa has been made, a systemic evaluation must be undertaken to pursue potential life-threatening involvement. If other organ systems are involved, the patient will need to undergo systemic therapy, and a multidisciplinary approach is required. The sensory nerves are almost always affected by mononeuritis multiplex. This leads to a peripheral neuropathy, and it is cited as the most common extracutaneous finding in polyarteritis nodosa. The kidneys, heart, and gastrointestinal tract are also routinely affected, and any of these can lead to life-threatening complications. Renal artery aneurysms can form along the branches of the renal artery and can become thrombosed. This leads to wedge-shaped infarcts in the kidney with varying amounts of kidney function loss. Gastrointestinal arterial infarcts can also cause bowel ischemia and symptoms of an acute abdomen. The central nervous system and the musculoskeletal system are also frequently affected.
 |
| Mononeuritis multiplex with polyarteritis nodosa |
Pathogenesis: The
pathomechanisms that incite polyarteritis nodosa are poorly understood.
Hepatitis-induced polyarteritis is believed to be partially caused by viral
disruption of arterial endothelial cells as a result of circulating antigen-antibody complexes.
Histology: Necrotizing
vasculitis of medium and small arteries in the deep reticular dermis is the
hallmark of polyarteritis nodosa. The inflammatory infiltrate is predominantly
made up of neutrophils with an admixture of other leukocytes. Fibrinoid
necrosis is prominent, and intraluminal clotting is often seen. Depending on
the type of skin lesion biopsied, varying amounts of skin necrosis are seen.
This is most commonly observed in areas of infarcted skin and ulceration.
Treatment: The first-line
therapy is with oral corticosteroids. The use of steroid-sparing agents early
in the course of the disease may help decrease steroid-induced side effects.
Cyclophosphamide is the major steroid-sparing agent used. Therapy for
polyarteritis nodosa induced by hepatitis B virus infection is targeted at the replicating viral particles.




