INTRACRANIAL
HEMORRHAGE IN THE NEWBORN
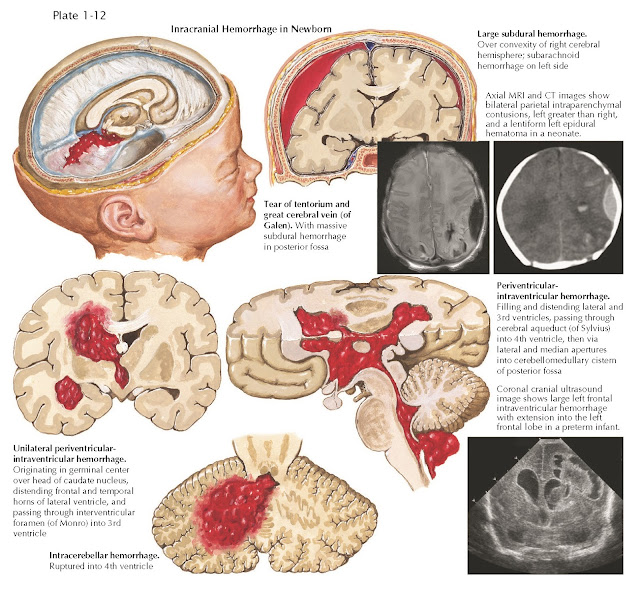
Intracranial hemorrhage in the neonate is classified by location and in order of frequency as (1) periventricularintraventricular, (2) subarachnoid, (3) subdural, or (4) posterior fossa hemorrhage. All neonates should be followed closely for symptomatic anemia.
Periventricular-intraventricular
hemorrhage (IVH) originates in
the germinal matrix near the lateral ventricles and typically is observed in
infants born preterm before 34 weeks’ gestation (Plate 1-12). In preterm infants, the inherent friability of the germinal
matrix is often complicated by cardiopulmonary compromise during birth and
physiologic stresses of adjusting to the extrauterine environment in the early
neonatal period. Massive bleeding, now quite rare, precipitates a bulging
fontanelle, respiratory difficulties, tonic posturing, seizures, anemia and, ultimately, multisystem
failure. Minor bleeding detected with serial cranial ultrasonography is now
more common. Some preterm infants will develop ventriculomegaly without cranial
growth or elevated intracranial pressure, consistent with hydrocephalus ex
vacuo from encephalomalacia. Approximately 15% of preterm infants with IVH will
require surgical intervention for symptomatic hydrocephalus. Long-term
neurologic deficits are common in preterm infants with IVH, including cerebral
palsy, epilepsy, cognitive delay, and behavioral abnormalities. In full- term
infants, IVH typically occurs secondary to deep central venous thrombosis, and
approximately half of these infants will develop early or late hydrocephalus.
Term infants with IVH are also prone to chronic neurologic deficits, including
epilepsy, cognitive delay, and behavioral abnormalities.
Subarachnoid hemorrhage may be caused by asphyxia or by forces of normal
delivery. In full-term infants, it may be
asymptomatic or associated with focal or generalized seizures, with no focal
deficits. Subdural hemorrhage results from tears in the falx cerebri and
tentorium, rupture of bridging veins over the hemispheres, or occipital
osteodiastasis in breech delivery. Causes include excessive molding forces
during delivery, the infant’s size, and difficult extractions. Symptoms are
acute or subacute hemiparesis, focal seizures, and ipsilateral pupillary
abnormalities. Surgical drainage is the appropriate treatment in select cases.
Cranial ultrasonography rarely provides adequate information, and either a
rapid computed tomography (CT) or MRI scan is needed for management decisions.
Posterior fossa hemorrhage can result from tentorial trauma or occipital
osteodiastasis. Either a rapid CT or MRI scan is needed for management
decisions; cranial ultrasonography does not provide adequate imaging to assess
the mass effect of the hematoma. Surgical drainage is rarely indicated.