THORACOLUMBAR SPINE TRAUMA
Most thoracic and lumbar fractures result from vertical compression or flexion-distraction injuries. These injuries frequently occur around the thoracolumbar junction (T11-L2), because it represents a transition from the stiffer thoracic to the more flexible lumbar spine. The upper thoracic region (T1-10) is more injury resistant because it is stabilized by the ribs, and the lower lumbar region (L3-5) has larger, stronger, and more injury-resistant vertebra.
Multiple classification systems exist for thoracolumbar trauma, but the
three-column theory of Denis is among the simplest to conceptualize (see Plate 1-28). This
concept divides the vertebral body into three columns: the anterior column
extending from the anterior longitudinal ligament through the anterior two
thirds of the vertebral body, the middle column containing the posterior third of
the vertebral body and posterior longitudinal ligament; and the posterior
column, which includes the posterior spinal elements (lamina, pedicles, spinous
processes) and posterior ligamentous complex (supraspinous and interspinous
ligaments, facet capsules, and ligamentum flavum). Injuries involving one
column can frequently be treated nonoperatively, two-column injuries may
require surgical management, and three-column injuries generally mandate
surgical stabilization and fusion.

THREE-COLUMN CONCEPT OF SPINAL STABILITY AND COMPRESSION FRACTURES
COMPRESSION FRACTURES
Compression fractures result from failure of the anterior vertebral
column when a flexion force is applied. This most commonly occurs at the
thoracolumbar junction in elderly patients with osteoporosis. It is
generally a stable fracture, and treatment is usually symptomatic with pain
medication, restricted activity, and a thoracolumbar orthosis for comfort. The
fracture typically becomes stable once the bone heals. Surgical treatment
involves cement augmentation of the vertebral body to provide immediate stability
and to minimize the risk of progressive kyphosis. Multiple compression
fractures in patients with severe osteoporosis can cause a kyphotic,
stooped posture (see Plate 1-28). In such cases, cement augmentation of
the fractured vertebra should be considered.
BURST FRACTURES
Burst fractures involve failure of the anterior and middle columns of
the spine from an axial load and are generally associated with higher-energy
trauma than simple
compression fractures. Because the posterior vertebral body (middle column) is
fractured, bony fragments can retropulse into the spinal canal and may cause
spinal cord or nerve root injury (see Plate 1-30). Suspected burst fractures
should be evaluated by CT or MRI to evaluate the degree of spinal canal
compromise and the integrity of the bony and ligamentous structures of the
posterior column. Posterior column injury denotes a more severe fracture
pattern (a “three-column” injury) that frequently requires surgery.
Treatment of burst fractures varies and has been the subject of some
controversy. Stable burst fractures without neurologic injury can be treated
with pain medication, activity restriction, and a thoracolumbar orthosis to
relieve pain and promote bony healing. Relative indications for surgery include
greater than 25 degrees of kyphosis, greater than 50% height loss of the
vertebral body, or greater than 50% spinal canal compromise. A complete or
incomplete neurologic injury and an injury to the posterior column (a
three-column injury) constitute absolute indications for surgery. Surgery
typically involves instrumented spinal fusion two levels above and two levels
below the fractured vertebra. If there is a neurologic injury, then a
decompression is also performed. Posterior-only procedures can be performed
when there is no need for decompression of bony fragments within the spinal
canal, such as when there is no neurologic injury. It can also be performed in
patients requiring decompression with an acute fracture (<5 days after injury)
because such fracture fragments are mobile and can usually be reduced by a
combination of distraction and lordosis. Anterior procedures are appropriate
for subacute injuries requiring decompression, in patients with a
severe neurologic deficit and significant canal intrusion by fracture
fragments, and in patients with severely comminuted vertebral body fractures
with no anterior column support (see Plate 1-30).

COMPRESSION FRACTURES (CONTINUED)
CHANCE FRACTURES
A Chance fracture is typically a bony injury through the vertebra in the
thoracolumbar spine. It is best visualized on the lateral
radiograph or CT scan. The Chance fracture is also known as a “seat belt”
fracture, because it frequently results from motor vehicle accidents in which
the patient wears a lap belt without a shoulder belt. With sudden deceleration,
the patient simultaneously experiences flexion anteriorly, with the lap belt
acting as the pivot point, and distraction (tension) of the posterior column of
the spine. As the distraction continues, a fracture propagates from posterior
to anterior through the spine, involving all three columns (see
Plate 1-30). Although the fracture often reduces
spontaneously, it is inherently unstable. Fractures must be treated surgically
or immobilized in a thoracolumbar orthosis (with spinal stability verified with
a standing radiograph in the brace). Occasionally, this flexion-distraction
injury affects only the discoligamentous structures in the spine, resulting in
a “soft tissue Chance” injury. In this variant of the injury, the transverse
cleavage plain propagates through the posterior ligamentous complex
(supraspinous and interspinous ligaments, ligamentum flavum, and facet
capsules) and anteriorly through the intervertebral disc. Signs of this injury
on the lateral radiograph include gapping at the facet joint and widening of
the distance between spinous processes. This injury must be treated by spinal
fusion because these discoligamentous structures will not spontaneously heal
after being disrupted.
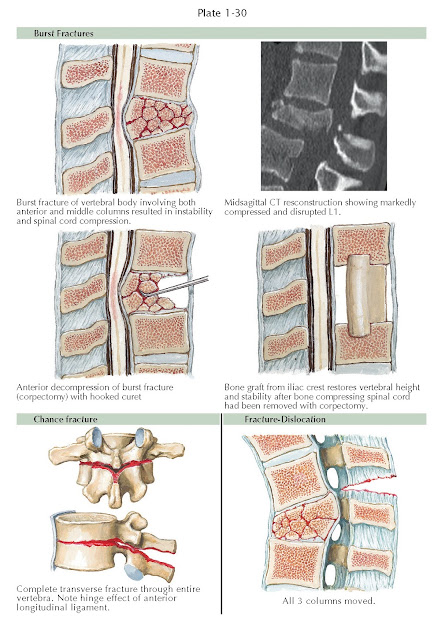
BURST, CHANCE, AND UNSTABLE FRACTURES
UNSTABLE INJURIES OF THE THORACOLUMBAR SPINE
The thoracolumbar junction is vulnerable to several different mechanisms
of injury: flexion, rotation, axial loading, or any combination of those
forces. Fracture- dislocations are relatively common in this region, where the
less mobile thoracic spine meets the highly mobile segments of the lumbar
spine. A fracture-dislocation of the thoracolumbar spine is severe and involves
disruption of all three columns of the spine (see Plate 1-30). These fractures
are inherently unstable and are associated with a high rate of neurologic
injury. Treatment of these injuries typically involves instrumented spinal
fusion and is directed at restoring stability to this area.
SACRAL FRACTURES
Traumatic sacral fractures can present as a solitary injury but often
are observed in association with a pelvic ring or lumbosacral facet injuries in
a patient with multiple injuries. The closer the fracture is to the
midline (either involving the sacral neural foramina or central canal), the
higher is the rate of neurologic injury. Most sacral fractures are stable and
do not require surgery. In patients with neurologic injury and objective
evidence of neurologic compression, however, surgical decompression and
stabilization may be indicated.




