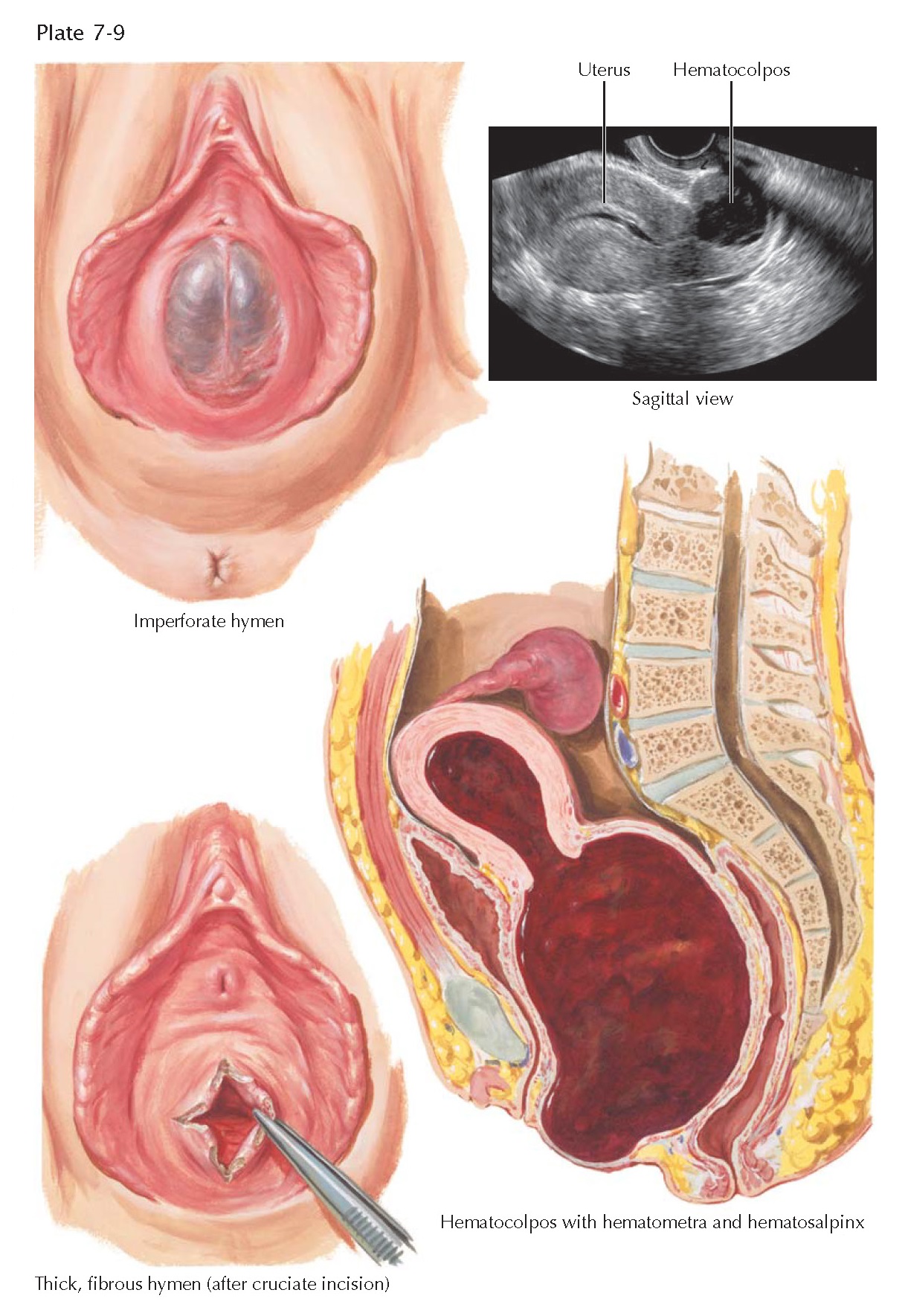
IMPERFORATE HYMEN, HEMATOCOLPOS, FIBROUS
HYMEN
An imperforate hymen is the most commonly encountered anomaly resulting from abnormalities in the development or canalization of the müllerian ducts. It is caused by failure of the endoderm of the urogenital sinus and the epithelium of the vaginal vestibule to fuse and perforate during embryonic development. In addition to primary amenorrhea and coital dysfunction, an imperforate hymen may also be associated with endometriosis, vaginal adenosis, infertility, chronic pelvic pain, long-term sexual dysfunction, and hematocolpos. The hymen, located at the junction of the vagina and the vestibule, is the product of the combined embryo- logic fusion of the urogenital sinus and the müllerian ducts. As the urogenital sinus advances upward like a diverticulum from the outside, it envelops the column of müllerian cells, which has already moved nearly four-fifths of the distance from the cervix down to the vestibule. The infoldings of the sinus at the point of union form the lateral walls of the hymen, but the posterior or dorsal portion is a composite of sinus cells externally and müllerian cells internally. The superficial epithelium of the hymen, as of the vagina and cervical portio vaginalis, is derived entirely from the epithelium of the urogenital sinus, which pushes up the vaginal tube and undergoes differentiation into the stratified squamous layer. The opening of the vagina may occur independently of the formation of the hymen.
It is obvious that the complexity of this embryologic development may
lead to congenital hymenal malformations. The imperforate hymen is usually
detected at birth or puberty. At birth, a hydromucocolpos may accumulate under
the influence of maternal hormones. Hence, at birth a bulging of the imperforate
hymen may be noted between the labia, especially when there is an increase in
intraabdominal pressure such as seen during crying. If there is a significant
hydromucocolpos detected by rectal examination in the newborn, then the hymen
should be excised (cruciate incision followed by excision of margins) to allow
continued drainage. During childhood, the imperforate hymen may be asymptomatic
prior to puberty and may go unrecognized unless detected by careful physical
examination. However, with the beginning of menstruation and the entrapment of
menstrual flow, the vagina gradually becomes distended with blood. From the
pressure of retained blood within the vagina, the hymen bulges outward. As seen
in the cross section, this situation may progress to the extreme, with the
entire vagina engorged with old blood (hematocolpos), the uterus likewise
enlarged by its own retained menstrual flow (hematometra), and blood passing
through the tubal isthmus to form a large hematosalpinx, which occasionally
drains into the peritoneal cavity. Because of the possible impact on the upper
genital tract, ultrasonography to evaluate the
upper genital tract is often indicated. These patients may seek medical
assistance because of primary amenorrhea, pelvic pain (especially cyclic), a
pelvic mass, or occasionally urinary retention with large masses. Incision with
excision of the margins of the hymen and release of the retained blood quickly
relieves the situation. Occasionally, the atresia involves not only the hymen
but also the lowermost portion of the vagina and, in these patients, a somewhat
deeper dissection must be done before the hematoma can be evacuated.
A different form of external vaginal atresia is a thick, fibrous, but not
imperforate hymen, which can easily be incised to produce normal patency of the
vaginal canal. This type of hymen, although much discussed by lay-persons and feared by the unmarried girl, is
relatively uncommon. When it occurs, it may cause dyspareunia. Although
properly considered an anomaly, this malformation, unlike those of the upper
vagina, is usually not associated with congenital anomalies elsewhere in the genitourinary
tract.