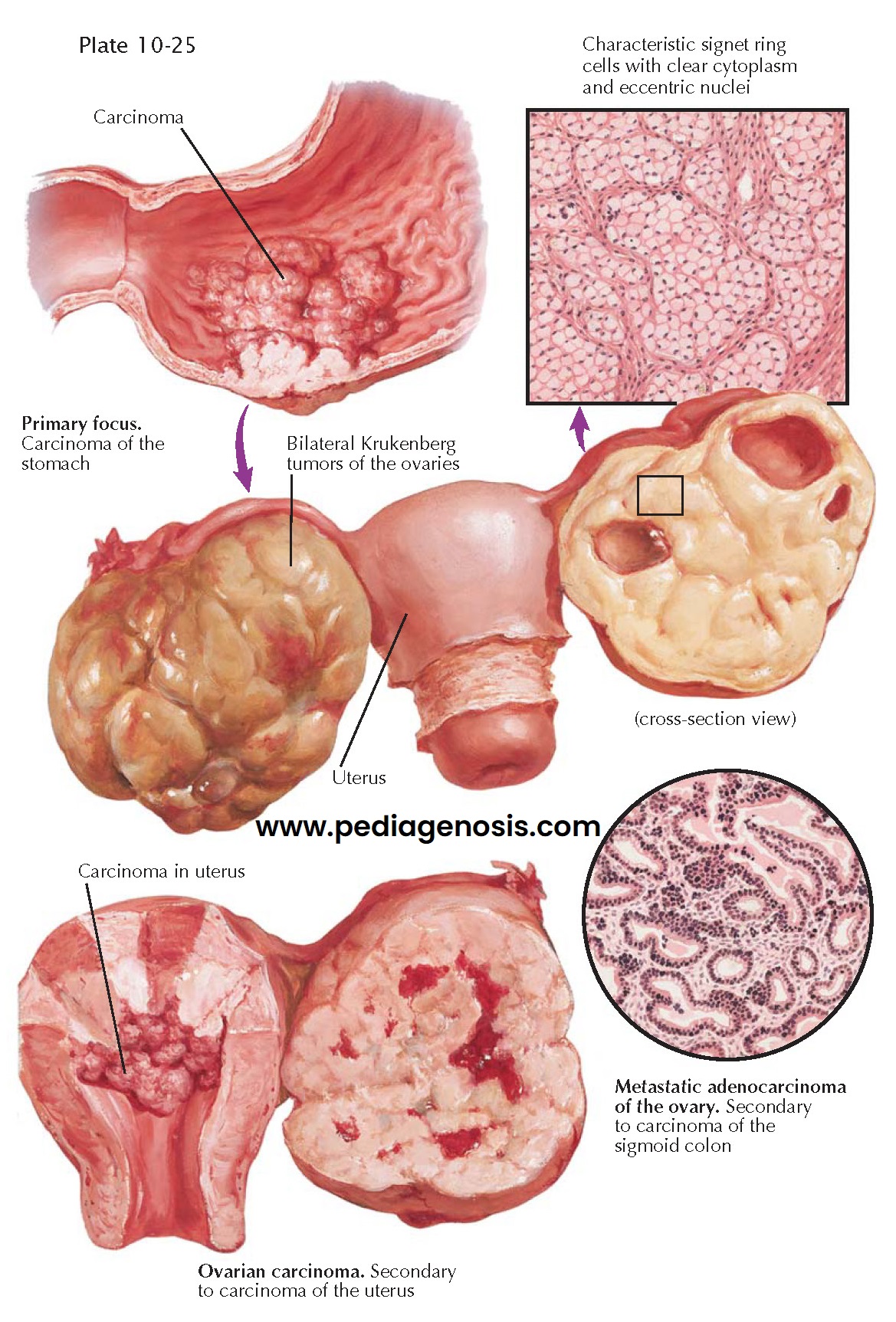
SECONDARY OVARIAN CARCINOMA
Metastatic cancer of the ovary accounts for only about 5% of ovarian cancer. The ovary is particularly prone to metastatic invasion by carcinoma. The primary sites include the breast, stomach, small and large intestine, appendix, liver, gallbladder, bile ducts, pancreas, uterus, tubes, opposite ovary, bladder and ureters, lungs, and meninges. Frequently, metastases are from primary tumors that originate elsewhere in the female reproductive tract, particularly from the endometrium and fallopian tube. Secondary ovarian carcinoma is most frequently seen from the fourth to the sixth decades of life. The ovaries are bilaterally involved in 66% to 75% of cases. Ascites is often evident (50%). The ovarian neoplasms may be asymptomatic or may manifest symptoms and signs similar to those produced by primary ovarian carcinoma. In the presence of a known primary lesion and palpable enlargement of the ovaries, the diagnosis of secondary carcinoma may reasonably be suspected. Similarly, the discovery of bilateral, solid ovarian growths on pelvic examination is an indication for a thorough search for a primary source elsewhere. Esophagoscopy, gastroscopy, sigmoidoscopy, or colonoscopy should be considered as a part of the evaluation when a gastrointestinal source is being sought.
In fully half of the cases, the ovarian lesion may not be detectable
grossly. The tumors may be minute or enlarged to diameters of 20 to 30 cm. The
general contour of the ovary is usually retained. The typical secondary ovarian
carcinoma is of moderate size, oval or kidney shaped, smooth or lobulated, firm,
grayish white in color, with a well-developed capsule and little tendency
toward adhesions. Depending upon the presence of necrosis, cystic degeneration,
hemorrhage, myxomatous changes, and the degree of connective tissue
proliferation, the cut surface may be firm, spongy, partly cystic, or gelatinous
and grayish white or yellow in color, with hemorrhagic areas of red or brown.
The histologic picture is generally similar to that of the primary
lesion. The anaplastic, epithelial elements may appear as clusters of acini,
cords, masses, or sheets, with varying degrees of mucoid change. The stroma may
be abundant or sparse, cellular, edematous, and myxomatous.
The Krukenberg tumor refers to a secondary ovarian carcinoma that
manifests marked proliferation of the connective tissue elements, sarcoma-like
areas, epithelial anaplasia, and mucoid epithelial and myxomatous changes.
Krukenberg tumors are the third most common metastatic ovarian cancer (after
epithelial and germ-cell tumors) and make up 14% of these cancers. Unlike some
forms of cancer, there is no racial bias. Signet-ring cells, in which the
nucleus is flattened to one side by secretion distending the cell, are
characteristic. The most common site of origin is the stomach or large
intestine, though metastatic breast cancer may appear similar histologically.
Metastatic tumors from the gastrointestinal tract to the ovary can be
associated with sex hormone production, usually estrogen. A few cases of
Krukenberg tumors have been described with no apparent distant primary
malignancy, suggesting the rare possibility of a primary ovarian tumor with the
histologic features of a Krukenberg tumor.
Debate exists over the exact mechanism of metastasis of the tumor cells
from the gastrointestinal tract to the ovaries; classically, it was thought
that direct seeding across the abdominal cavity accounted for the spread of
this tumor, but some have suggested that lymphatic or hematogenous spread is
more likely, as most of these tumors are found in the ovarian parenchyma and
not the surface.
The prognosis in secondary ovarian carcinoma is extremely grave, with 5-year survival unlikely. Progression and spread of the primary tumor are generally well under way when the ovarian sites are discovered. If widespread metastases are evident, surgery is not indicated. If the diagnosis is confirmed on laparotomy, a total hysterectomy and bilateral salpingo-oophorectomy may make the patient temporarily more comfortable.