ANATOMY OF THE KNEE
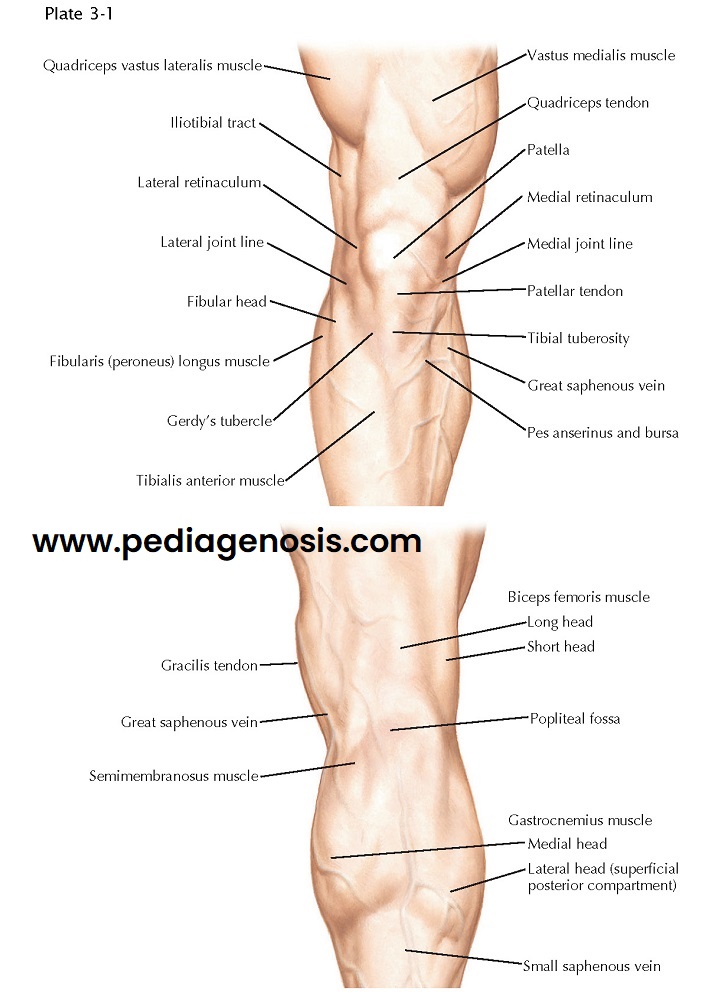
TOPOGRAPHIC ANATOMY OF THE KNEE
The knee is primarily a hinge joint that permits flexion and extension. In flexion, there is sufficient looseness to allow a small amount of voluntary rotation; in full extension, some terminal medial rotation of the femur (conjunct rotation) achieves the close-packed position. The condyles of the femur provide larger surfaces than those of the tibial condyles, and there is a component of rolling and gliding of the femoral surfaces that uses up this discrepancy. As the extended position is approached, the smaller lateral meniscus is displaced forward on the tibia and becomes firmly seated in a groove on the lateral femoral condyle, which tends to stop extension. However, the medial femoral condyle is still capable of gliding backward, thus bringing its flatter, more anterior surface into full contact with the tibia. These movements of conjunct rotation bring the cruciate ligaments into a taut, or locked, position. The collateral ligaments become maximally tensed, and a full, close-packed, and stable position of extension results. The tension of the ligaments and the close approximation of the flatter parts of the condyles make the erect position relatively easy to maintain.
The sequence of actions in flexion is reversed in
extension. Flexion can be carried through about 130 degrees and is finally
limited by contact between calf and thigh. The
muscles concerned in the movements at the knee are primarily thigh muscles.
There are three articulations in the knee—the
femoropatellar articulation and two femorotibial joints. The latter two are
separated by the intra-articular cruciate ligaments and the infrapatellar
synovial fold. The three joint cavities are connected by restricted openings.
The articular surfaces of the femur are its medial and
lateral condyles and the patellar surface, also known as the trochlea of the knee. The condyles are shaped like
thick rollers diverging inferiorly and posteriorly. Their surfaces gradually
change from a flatter curvature anteriorly to a tighter curvature posteriorly
and are separated from the patellar surface by a slight trochlear groove.
On the superior surface of the tibia, or the tibial
plateau, there are two separate, cartilage-covered areas. The surface of the
medial condyle is larger, oval, and slightly
concave; that of the lateral condyle is ap- proximately circular, concave from
side to side, but concavoconvex from before backward. The fossae of the
articular surfaces are deepened by disclike menisci. The composition and
morphology of the menisci make them important in distribution of load about the
knee during weight bearing.
 |
| OSTEOLOGY OF THE KNEE |
The articular capsule of the knee joint is scarcely
separable from the ligaments and aponeuroses apposed to it. Posteriorly, its vertical fibers arise from the condyles and
intercondylar fossa of the femur; inferiorly, these fibers are overlain by the
oblique popliteal ligament. The capsule attaches to the tibial condyles and,
incompletely, to the menisci. The external ligaments reinforcing the capsule
are the fascia lata and the iliotibial tract; the medial patellar and lateral
patellar retinacula; and the patellar, oblique popliteal, and arcuate popliteal
ligaments. The medial (tibial) collateral ligament also closely reinforces the
capsule on the medial side.
The aponeurotic tendons of the vastus muscles attach
to the sides of the patella and then expand over the front and sides of the
capsule as the medial and lateral patellar retinacula. Below, they insert into
the front of the tibial condyles and into their oblique lines as far to the
sides as the collateral
ligaments. Superficially, the fascia lata overlies and blends with the
retinacula as it descends to attach to the tibial condyles and their oblique
lines. Laterally, the iliotibial tract curves forward over the lateral patellar
retinaculum and blends with the capsule anteriorly. Its posterior border is
free, and fat tends to be interposed between it and the capsule.
The patellar ligament is the continuation of the
quadriceps femoris tendon to the tuberosity of the tibia.
An extremely strong and relatively flat band, it
attaches above the patella and continues over its front with fibers of the
tendon, ending somewhat obliquely on the tibial tuberosity. A deep
infrapatellar bursa intervenes between the tendon and the bone. A large,
subcutaneous infrapatellar bursa is developed in the tissue over the ligament.
The oblique popliteal ligament is one of the
specializations of the tendon of the semimembranosus muscle, which
reinforces the posterior surface of the articular capsule. As this tendon
inserts into the groove on the posterior surface of the medial condyle of the
tibia, it sends this oblique expansion lateralward and superiorly across the
posterior aspect of the capsule.
KNEE: LATERAL AND MEDIAL VIEWS
COLLATERAL LIGAMENTS
These ligaments prevent hyperextension of the joint
and any abduction-adduction angulation of the bones because they are essential
in resisting varus and valgus forces to the knee. Both collateral ligaments are
tighter in extension and progressively relaxed as the knee is brought into
flexion. The inferior genicular blood vessels pass between them and the capsule
of the joint, but only the lateral (fibular) collateral ligament stands clearly
away from the capsule.
The medial (tibial) collateral ligament is a strong,
flat band that extends between the medial condyles of the femur and tibia. It
can be broken down into superficial and deep layers that may be separated by a
thin bursa that facilitates the slight movement between these layers. The
medial collateral ligament (MCL) is well defined anteriorly, blending with the
medial patellar retinaculum. The pes
anserinus tendon overlies the ligament below, the two being separated by the
anserine bursa. The posterior portion of the ligament is characterized by
obliquely running fibers, which converge at the joint level from above and
below and give the ligament an attachment into the medial meniscus. The principal
inferior attachment of the ligament is about 5 cm below the tibial articular
surface immediately posterior to the insertion of pes anserinus.
The lateral (fibular) collateral ligament is a more
rounded, pencil-like cord, which is entirely separate from the capsule of the
knee joint. It is attached to a tubercle on the lateral condyle of the femur
above and behind the groove for the popliteus muscle. It ends below on the
lateral surface of the head of the fibula, about 1 cm anterior to its apex. The
tendon of the popliteus muscle passes deep to the ligament, and the biceps
femoris tendon divides around its fibular attachment, with a
small inferior subtendinous bursa intervening. Another bursa lies under the
upper end of the ligament, separating it from the popliteus tendon. The
synovial membrane of the joint, protruding as the subpopliteal recess,
separates the popliteus tendon from the lateral meniscus.
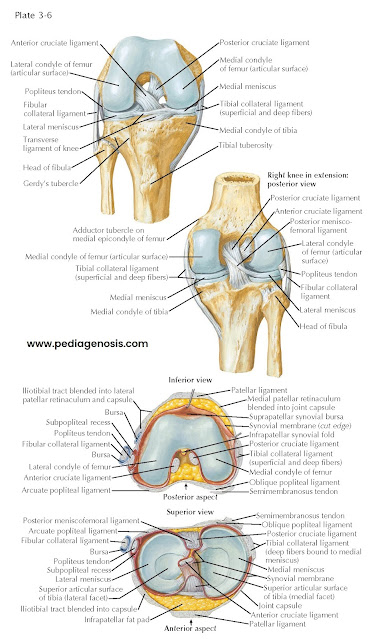
CRUCIATE LIGAMENTS
The cruciate ligaments prevent forward or backward
movement of the tibia under the femoral condyles. These ligaments also play a
large role in providing rotator stability about the knee joint. They are some-
what taut in all positions of flexion but become tightest in full extension and
full flexion. They lie within the capsule of the knee joint, in the vertical
plane between the condyles, but are excluded from the synovial cavity by
coverings of synovial membrane. Both ligaments spread linearly at their bony
attachments, especially at the femoral condyles.
The anterior cruciate ligament (ACL) arises from the
rough, nonarticular area in front of the intercondylar eminence of the tibia
and extends upward and backward to the posterior part of the medial aspect of
the lateral femoral condyle. The
ACL can be divided into an anteromedial bundle and a posterolateral bundle. The
anteromedial bundle is tight in flexion, and the posterolateral bundle is tight
in extension.
The thicker and stronger posterior cruciate ligament
(PCL) passes upward and forward on the medial side of the anterior ligament. It
extends from an extra-articular attachment over the back of the tibial plateau
to the lateral side of the medial condyle of the femur. The PCL also consists
of an anterolateral bundle and a posteromedial
bundle. The posteromedial bundle is tight in extension, and the anterolateral
band is tight in flexion. Both ligaments receive their primary blood supply
from the medial genicular artery and their innervations from branches off the
tibial nerve.
 |
| KNEE: POSTERIOR AND SAGITTAL VIEWS |
MENISCI
These crescent-shaped wafers of fibrocartilage sur-
mount the peripheral parts of the articular surfaces of the tibia. Thicker at their external margins and tapering to thin,
unattached edges in the interior of the articulation, they deepen the articular
fossae for the reception of the femoral condyles. They are attached to the
outer borders of the condyles of the tibia and at their ends, anterior and
posterior, to its intercondylar eminence.
The medial meniscus is larger and more nearly oval in
outline. Broader posteriorly, it narrows anteriorly as it attaches in the
intercondylar area of the tibia in front of the origin of the PCL. The lateral
meniscus is more nearly circular. Although smaller than the medial meniscus, it
covers a somewhat greater proportion of the tibial surface. Anteriorly, it
attaches in the anterior intercondylar area, lateral to and behind the end of
the ACL. Posteriorly, it ends in the posterior intercondylar area in front of
the end of the medial meniscus. The medial meniscus is also attached to the
MCL, making it significantly less mobile than the lateral meniscus. The lateral
meniscus is weakly attached around the margin of the lateral tibial condyle and
lacks an attachment where it is crossed and notched by the popliteus tendon. At
the back of the joint, it gives origin to some of the fibers of the popliteus
muscle; and close to its posterior attachment to the tibia, it frequently gives
off a collection of fibers, known as the posterior menisco- femoral ligament.
This may join the PCL or may insert into the medial femoral condyle behind the
attachment of the PCL. An occasional anterior meniscofemoral ligament has a
similar but anterior relationship to the PCL. The transverse ligament of the
knee connects the anterior convex margin of the lateral meniscus to the
anterior end of the medial meniscus.
The blood supply to the medial and lateral menisci
come from the superior and inferior branches of the medial and lateral
geniculate arteries, respectively. There are three commonly referred to zones
of the menisci based on their respective blood supply. Starting from the most
vascularized peripheral (outermost) portion of the meniscus, these are the
red-red, red- white, and white-white zones. These zones play a large role in
therapeutic decision making owing to the
role that increased vascularity will play in the likelihood of healing.
Vascularity is also variable among patients of different ages, because you ger
patients tend to have a more robust
blood supply.
KNEE: INTERIOR VIEW AND CRUCIATE AND COLLATERAL LIGAMENTS
SYNOVIAL MEMBRANE AND
JOINT CAVITY
The articular cavity of the knee is the largest joint
space of the body. It includes the space between and around the condyles,
extends upward behind the patella to include the femoropatellar articulation,
and then communicates freely with the suprapatellar bursa between the
quadriceps femoris tendon and the femur. The synovial membrane lines the
articular capsule and the suprapatellar bursa. Recesses of the joint cavity are
also lined by synovial membrane; the subpopliteal recess has been described.
Other recesses exist behind the posterior part of each femoral condyle; at the
upper end of the medial recess, the bursa under the medial head of the
gastrocnemius muscle may open into the joint cavity.
The infrapatellar fat body or pad represents an
anterior part of the median septum, which, with the cruciate ligaments,
separates the two femorotibial articulations. From the medial and lateral
borders of the articular surface of the patella, reduplications of synovial
mem- brane project into the interior of the joint and form two fringelike alar
folds, which cover collections of fat. The fat pad is a normal structure but in
many cases it may become inflamed or impinge within the patella and femoral condyle
and become problematic.
BLOOD VESSELS AND NERVES
In the region of the knee there is an important
genicular anastomosis. This consists of a superficial plexus above and below
the patella, plus a deep plexus on the capsule of the knee joint and the adjacent
bony surfaces. The anastomosis is made up of terminal interconnections of 10
vessels. Two of these descend into the joint—the descending branch of the
lateral circumflex femoral artery and the descending genicular branch of the
femoral artery. Five are branches of the popliteal artery at the level of the
knee—the medial superior genicular, lateral superior genicular, middle
genicular, medial inferior genicular, and lateral inferior genicular arteries.
Three branches of leg arteries ascend to the anastomosis—the posterior tibial
recurrent, circumflex fibular, and anterior tibial recurrent arteries. Veins of
the same names accompany the arteries. The lymphatics of the knee joint drain
to the popliteal and inguinal node groups.
The nerves of the knee joint are numerous.
Articular branches of the femoral nerve reach the knee via the nerves to the
vastus muscles and the saphenous nerve. The posterior division of the obturator
nerve ends in the joint, and there are also articular branches of the tibial
and common peroneal nerves.
PATELLA
The large sesamoid is developed in the tendon of the
quadriceps femoris muscle. It bears against the anterior articular surface of
the inferior extremity of the femur and, by holding the tendon off the lower
end of the femur, improves the angle of approach to the tendon to the tibial
tuberosity. The convex anterior surface of the patella is striated vertically
by the tendon fibers. The superior border is thick, giving attachment to the
tendinous fibers of the rectus femoris and vastus intermedius muscles. The
lateral and medial borders are thinner; they receive the fibers of the vastus
lateralis and vastus medialis muscles. These borders converge to the pointed
apex of the patella, which gives attachment to the patellar ligament. The articular surface is a smooth oval area,
divided by a vertical ridge into two facets. The ridge occupies the groove on
the patellar surface of the femur, the medial and lateral facets corresponding
to facing surfaces of the femur. The lateral facet is broader and deeper than
the medial. Inferior to the faceted area is a rough nonarticular portion from
which the lower half of the patella ligament arises.
The patella maintains a shifting contact with the
femur in all positions of the knee. As the knee shifts from a fully flexed to a fully extended position, first the superior,
then the middle, and lastly the inferior parts of the articular surface of the
patella are brought into contact with the patellar surfaces of the femur. The
largest amount of contact between the patella and the trochlea is at about 45
degrees of knee flexion.
Ossification develops from a single center, which appears early in the third year of life. Complete ossification occurs by age 13 in the male and at about age 10 in the female.