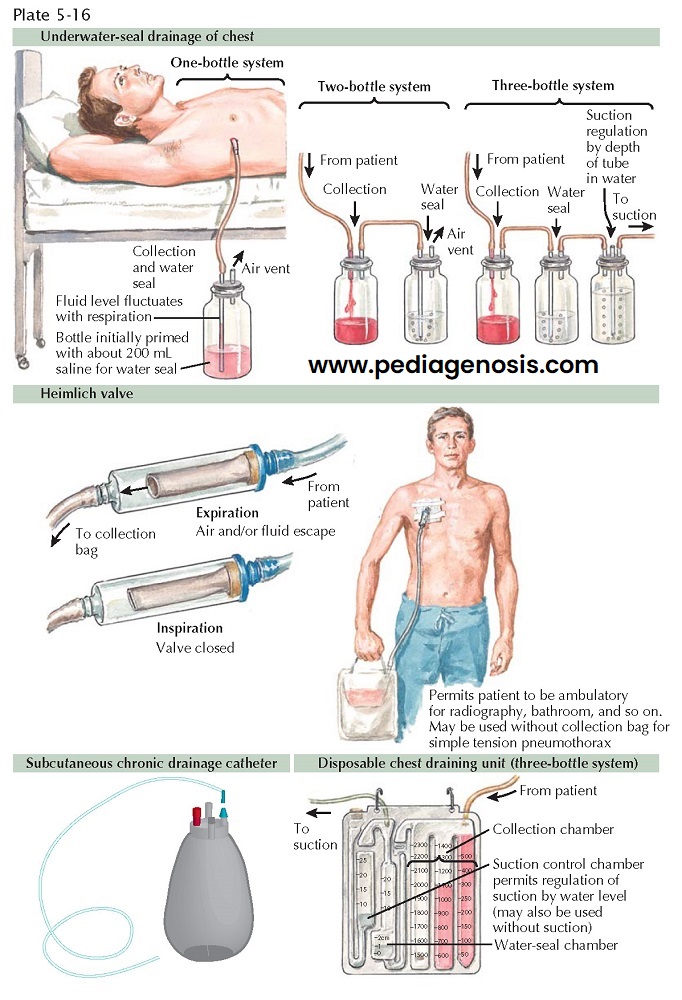
CHEST-DRAINING METHODS
After an intercostal tube has been inserted, the pleural contents are evacuated into a chest drainage system. In the case of a pneumothorax, a one-way flutter valve (i.e., Heimlich valve) can also be used. The essential feature of the system is a means to permit escape of gas or fluid from the pleural space with no possibility of return using gravity or suction.
In recent years, disposable suction systems have
become extremely popular, and some manufacturers have miniaturized these
systems for true portability. It is important to understand the evolution of
the now standard disposable suction systems. Initial drainage systems consisted
of one bottle to drain fluid and act as a water-seal chamber. The water-seal
chamber acts as a “pop-off” valve, preventing tension pneumothorax by allowing
intrapleural air to leave the chest. When there is communication between airway
opening (the mouth) and the pleural space, as in the case of a bronchopleural
fistula, bubbles can be seen in the water-seal chamber of the chest tube. A
drawback of the one-bottle system is that as drainage of fluid persisted, the
increasing height of the fluid column increased the resistance for the
evacuation of air. The two-bottle system separated the collection bottle from
the water-seal bottle. By adding a third bottle, suction to the patient is
regulated by the depth of the tube open to the atmosphere under water. As wall
suction is increased, the meniscus drops until it reaches the bottom of the
tube, and atmospheric air is then entrained. The disposable units incorporate
these three bottles into one plastic container. When it is intended that the
chest tube be connected to suction, one should always see bubbling in the
suction chamber. Again, bubbling in the water-seal chamber indicates an air
leak (communication between the airway opening and the pleural space) or a leak
in the system. Some new disposable units are “dry,” that is, suction is
observed when a float is seen in the appropriate window.
If evacuation of fluid or air is impeded, there is a
progressive increase in intrapleural pressure and further respiratory and
circulatory compromise. This may occur in a number of ways. Soft chest drainage
tubing may be occluded by kinking or outside pressure, or it may be of
insufficient diameter to drain a large air leak. Dependent loops of tubing
outside of the chest may contain fluid and result in significant back pressure
and accumulation of intrapleural fluid or air. More than one drainage tube may
be needed, especially in the case of larger air leaks.
In the case of pleural effusions, or in a patient who
has had a recent pleurodesis, the chest tube can usually be removed when
there is less than 100 to 200 mL of serous fluid draining in a 24-hour period.
Occasionally, serosanguineous fluid may leak through the hole from which a tube
has been removed, especially after coughing. This is not of concern because the
leak almost always ceases spontaneously. If drainage occurs around a tube that
is still in place, it suggests that the tip is no longer in communication with
the intrapleural fluid, and needs to be stripped of fibrinous material, flushed with sterile
saline, or removed. Infection caused by the presence of a drainage tube in the
pleural space is unusual as long as sterile technique was used during
insertion.
In certain situations, a tunneled, subcutaneous chest drain may be inserted to provide drainage of effusions for palliation. These devices allow patients to go home and can relieve symptoms of shortness of breath and chest pressure caused by chronic effusions.