Diagnostic Aids in Gastric Disorders
Every
diagnostic evaluation must begin by taking a skilled history and performing a
physical examination, but additional aids are usually necessary to make a
definitive diagnosis that will provide a specific plan for effective treatment.
Following the history and physical examination, laboratory testing and
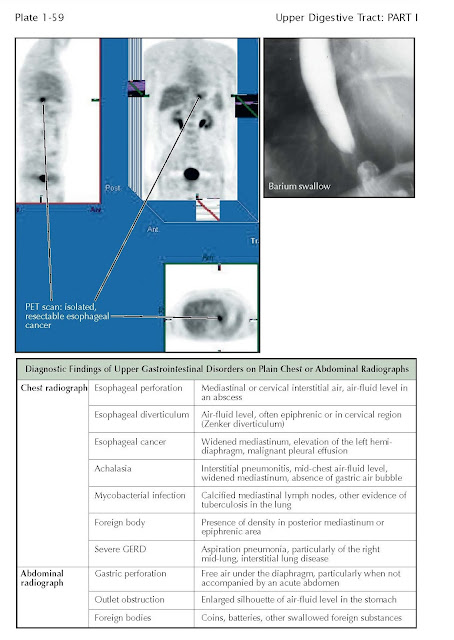
noncontrast chest or abdominal radiographs are often obtained. Common
radiographic findings on plain x-rays (no contrast agent administered) for
common upper digestive disorders are shown. The value of more precise imaging
technologies with endoscopic and radiographic studies is discussed with Plates
1-61 to 1-64 and of breath testing with Plates 1-65 and 1-66. An important
element of a thorough physical examination of a patient with symptoms of a
digestive disorder is evaluation of the stool for blood. Detecting blood from
the upper gastrointestinal tract using fecal occult blood testing with a
guaiac-based technology, while less specific, is more sensitive than fecal
immune testing for hemoglobin because the immunogenicity of a hemoglobin
molecule released in the esophagus or stomach can be degraded by pancreatic and
small intestinal digestive enzymes.
Physiologic testing of acid production and exposure and
of motility functions of the upper digestive tract is a commonly used,
invaluable tool. Three types of esophageal and gastric pH monitoring are in
common use. The traditional esophageal pH study provided only a transnasal
24-hour study of reflux. It is time honored and safe and provides accurate
information about the severity of exposure of acid in both the esophagus and
stomach. Alternatively, an intraesophageal clip pH study can be
performed by placement of a pH electrode 5 cm above the gastroesophageal
junction using endoscopy. It has several advantages over the transnasal probe
because it is wireless and therefore does not have the inconvenience,
embarrassment, potential risk, and dis- comfort of the transnasal device. It
records, for 48 hours, the intraesophageal pH measures as the patient eats and
sleeps as usual; this can be a challenge with the transnasal device. The major
disadvantage of both devices, however, is that pH recordings only report the
severity of acid reflux. A major advance over both of these techniques is high-resolution
manometry and the impedance reflux study. High-resolution manometry is
performed with a probe that has multiple recording electrodes, permitting a
more rapid and accurate evaluation of esophageal motility testing throughout
the length of the esophagus, without the annoyance of moving the device. More
importantly, the impedance technology permits the evaluation of both acid and
nonacid reflux and fluid dwell time and a correlation between manometry and
bolus transit. This device is limited by recording for only 24 hours and by placement
of the catheter transnasally, but the increased accuracy and extensive
diagnostic information provided coupled with the very small diameter of the
device make it the procedure of choice for esophageal motility and reflux
studies.
Physiologic testing of gastric motility and pH physiology
are also commonly performed. Gastric motility is most commonly evaluated after
a patient has eaten a meal of radio-labeled liquids and solids in the nuclear
medicine department of a hospital or an outpatient facility. The test
involves little radiation, is easy to perform, and has essentially no risk for
the patient. The wide variability in normal emptying rates may affect the
results, however, as may a patient’s mood and overall health, which may also
cause emptying times to vary widely (poor reproducibility). This has led to the
recommendation that recordings be made for a minimum of 4 hours and that a
standardized meal be eaten. Alter-natively, gastric motility functions can be
evaluated, along with small bowel motility, by means of a capsule motility test.
The capsule can be swallowed by a patient in the
office, and recordings are made as the patient goes about normal activities.
Gastric secretory physiology is most commonly evaluated
by a basal rate and then by a stimulated, titratable gastric secretory rate.
This test is very important in the evaluation of acid secretion in patients who
may have Zollinger-Ellison syndrome or other causes of hypergastrinemia. Gastric
acid secretory studies are described in greater detail with Plates 4-27 and 4-36.