Heart Anatomy
The heart, enclosed in pericardium,
occupies the middle mediastinum. It is roughly cone-shaped and lies behind the
sternum with its base facing posteriorly and its apex projecting inferiorly,
anteriorly and to the left, producing the cardiac impression in the left lung.
 |
| Fig. 2.31 Transverse CT image at the level of the eighth thoracic vertebra. |
 |
Fig.
2.32 Borders and valves of the heart and their relationships to the anterior
chest wall.
Borders
It is useful to represent the outline
of the heart as a projection onto the anterior chest wall. When represented in
this way, the heart has right, inferior and left borders (Fig.
2.32). The right border is
formed by the right atrium and runs between the third and sixth right costal
cartilages approximately 3 cm from the midline. The inferior border is formed
mainly by the right atrium and right ventricle. At its left extremity, the
border is completed by that part of the left ventricle which forms the apex of
the heart. The inferior border runs from the sixth right costal cartilage
approximately 3 cm from the midline to the apex, which usually lies behind the
fifth left intercostal space, 6 cm from the midline. In the living, the apex
usually produces an impulse (apex beat) palpable on the anterior chest wall.
The left ventricle together with the left auricle (left atrial appendage) form
the left border of the heart, which slopes upwards and medially from the apex
to the second left intercostal space, approximately 3 cm from the midline.
Most of the anterior surface of the
heart consists of the right atrium and right ventricle (Fig.
2.33). The left ventricle
contributes a narrow strip adjacent to the left border of the heart. The
anterior surface is completed by the right and left auricles. The coronary
sulcus descends more or less vertically on the anterior surface and contains
the right coronary artery embedded in fat. The anterior surfaces of the right
and left ventricles are separated by the anterior interventricular artery (left
anterior descending artery).
Most of the inferior (diaphragmatic)
surface of the heart (Fig. 2.34) consists of the two ventricles, the left usually
contributing the greater area. The posterior interventricular vessels mark the
boundary between these two chambers. The surface is completed by a small
portion of the right atrium adjacent to the termination of the inferior vena
cava.
The posterior surface or base of the heart
(Fig. 2.35) consists mostly of the left atrium together with a small part of
the right atrium.
 |
Fig. 2.33 Anterior surface of the heart.
 |
Fig. 2.34 Inferior surface of the heart. The inferior part of the
fibrous pericardium has been removed with the diaphragm.
 |
Fig.
2.35 The posterior surface of the heart showing the reflection of the serous
pericardium and the site of the oblique pericardial sinus.
Chambers
and valves
The cavities of the right and left
atria are continuous with those of their respective ventricles through the
atrioventricular orifices. Each orifice possesses an atrioventricular valve,
which prevents backflow of blood from the ventricle into the atrium. The
myocardium of the atria is separated from that of the ventricles by connective
tissue, which forms a complete fibrous ring around each atrioventricular
orifice. Interatrial and interventricular septa separate the cavities of the
atria and ventricles. Valves, each with three semilunar cusps, guard the
orifices between the right ventricle and pulmonary trunk (pulmonary valve) and
the left ventricle and ascending aorta (aortic valve). All these valves close
passively in response to differential pressure gradients.
The right atrium receives blood from
the superior and inferior venae cavae and from the coronary sinus and cardiac
veins, which drain the myocardium. The superior vena cava enters the upper part
of the chamber. Adjacent to its termination is a broad triangular
prolongation of the atrium, the auricle (atrial appendage), which overlaps the
ascending aorta (Fig. 2.36).
 |
Fig.
2.36 Interior of the right atrium and auricle, exposed by reflection and
excision of part of the anterior atrial wall.
Internally, the anterior wall of
the right atrium possesses a vertical
ridge, the crista terminalis (Fig. 2.36). From the crista, muscular ridges (musculi
pectinati) run to the left and extend into the auricle. The posterior
(septal) wall is relatively smooth but possesses a well-defined ridge
surrounding a shallow depression named the fossa ovalis. This fossa is the site
of the foramen ovale, which, in the fetus, allows blood to pass directly from
the right to the left atrium. The coronary sinus empties into the chamber close
to the atrioventricular orifice. Inferiorly, the right atrium receives the
inferior vena cava immediately after the vessel has pierced the central tendon
of the diaphragm. A fold called the valve of the inferior vena cava (Fig.
2.36) projects into the
chamber and is the remnant of a fetal structure that directed the flow of blood
across the right atrium towards the foramen ovale.
From the right atrium, blood flows
into the right ventricle through the right atrioventricular orifice, which is
guarded by the tricuspid valve (Fig. 2.37). The valve possesses three cusps, the bases of which attach to the margins of the atrioventricular
orifice, while their free borders project into the cavity of the right
ventricle (Fig. 2.38), where they are anchored by fibrous strands (chordae tendineae) to the
papillary muscles of the ventricle. During ventricular contraction (systole),
the papillary muscles pull on the chordae, preventing eversion of the valve
cusps and reflux of blood into the atrium. The valve lies in the midline behind
the lower part of the body of the sternum (Fig. 2.32) and its sounds are heard
best by auscultation over the xiphisternum.
 |
Fig.
2.37 Tricuspid valve, revealed after removal of the lateral wall of the right
atrium.
 |
Fig. 2.38 Interior of the right ventricle seen after removal of its
anterior wall.
|
Right ventricle
The right ventricle has the right
atrium on its right and the left ventricle both behind and to its left. The
chamber forms parts of the anterior and inferior surfaces of the heart and
narrows superiorly at the infundibulum, which leads into the pulmonary trunk (Fig.
2.38). The walls of the
right ventricle are thicker than those of the
right atrium and internally possess numerous muscular ridges called trabeculae
carneae (Fig. 2.43). One of these, the moderator band (Fig. 2.54), often
bridges the cavity of the chamber, connecting the interventricular septum to
the anterior ventricular wall. When present, it carries the right branch of the
atrioventricular bundle of conducting tissue (p. 56). Projecting from the
ventricular walls into the interior of the chamber are processes of myocardium,
the papillary muscles, each attached at its apex to several chordae tendineae.
The right ventricle is separated from the left ventricle by the
interventricular septum, which is muscular inferiorly and membranous superiorly
(Figs 2.43 & 2.46).
Pulmonary valve
The pulmonary orifice lies between the
infundibulum and the pulmonary trunk and is guarded by the pulmonary valve (Figs
2.39 & 2.40), which
consists of three semilunar cusps. The valve closes during ventricular
relaxation (diastole), preventing backflow of blood from the pulmonary trunk
into the right ventricle. The valve lies behind the left border of the sternum
at the level of the third costal cartilage (Fig. 2.32). Sounds generated by
this valve are loudest over the anterior end of the second left intercostal
space.
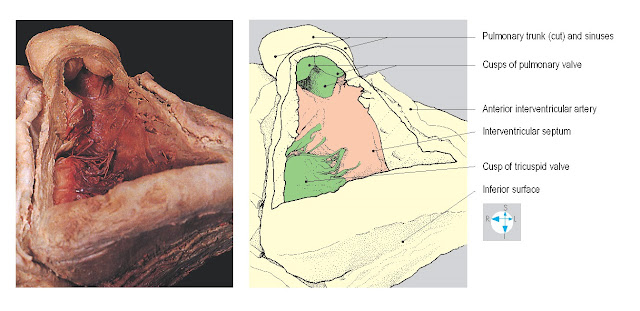 |
Fig. 2.39 Ventricular surfaces of the cusps of the pulmonary valve
seen after removal of part of the anterior wall of the right ventricle.
|
 |
Fig. 2.40 Pulmonary and aortic valves seen from above.
|
Left atrium
The left atrium lies behind the right
atrium and forms the base of the heart. It possesses a hook-like auricle (left
atrial appendage), which projects forwards to the left of the pulmonary trunk
and infundibulum. The chamber receives superior and inferior pulmonary veins
from each lung (Fig. 2.35). The four pulmonary veins, together with the two
venae cavae, are all enclosed in a sleeve of serous pericardium, forming the
superior limit of the oblique pericardial sinus. The left atrium forms the
anterior wall of this sinus, which separates the chamber from the fibrous
pericardium and oesophagus. Most of the inner surface of the left atrium is
smooth (Fig. 2.41), although musculi pectinati are present in the auricle.
Mitral (bicuspid) valve
The left atrium communicates
anteroinferiorly with the left ventricle through the left atrioventricular
orifice, which is guarded by the mitral valve. This valve possesses two cusps,
whose bases attach to the margins of the atrioventricular orifice (Fig.
2.41), while their free
borders and cusps are anchored by chordae tendineae to the papillary muscles
within the left ventricle (Fig. 2.42). The valve prevents reflux during ventricular
contraction. Although it lies in the midline at the level of the fourth costal
cartilages (Fig. 2.32), the sounds of the mitral valve are best heard over the apex
of the heart.
From the left atrioventricular
orifice, the left ventricle extends forwards and to the left as far as the
apex. The thickness of the wall of the chamber is normally three times that of
the right ventricle (Fig. 2.43). Internally, there are prominent trabeculae
carneae and papillary muscles (Fig. 2.46). The chamber narrows as it passes
upwards and to the right behind the infundibulum to form the aortic vestibule (Fig.
2.44), the part of the ventricle
that communicates with the ascending aorta through the aortic orifice.
Aortic valve
The aortic valve consists of three
semilunar cusps (Fig. 2.45), which prevent backflow of blood from the ascending
aorta during ventricular diastole. The valve lies behind the sternum to the
left of the midline at the level of the anterior end of the third left
intercostal space (Fig. 2.32). However, its sounds are best heard over the
medial ends of the first and second right intercostal spaces.
The pulmonary trunk and the ascending
aorta lie within the fibrous pericardium, enclosed together in a sleeve of
serous pericardium anterior to the transverse pericardial sinus (Fig. 2.40).
The pulmonary trunk extends upwards and backwards, while the ascending aorta
initially lies behind it and passes upwards and forwards, overlapped by the
right auricle. At the origin of each vessel are three dilatations or sinuses
(Figs 2.39 & 2.45), one immediately above each of the cusps of the pulmonary
and aortic valves. When ventricular contraction ceases, blood flows into the
sinuses, thus pushing against the cusps and closing the valves. Two of the
aortic sinuses give rise to the right and left coronary arteries.
The pulmonary trunk emerges from the pericardium
and divides into right and left pulmonary arteries in the concavity of the
aortic arch, anterior to the bifurcation of the trachea at the level of the
fourth thoracic vertebra. As the ascending aorta pierces the fibrous
pericardium, it turns backwards and to the left, becoming the arch of the
aorta.
Connecting the aortic arch to the
pulmonary trunk (or to the commencement of the left pulmonary artery) is the
ligamentum arteriosum (Fig. 2.46), the remnant of the fetal ductus arteriosus
which conveyed blood from the pulmonary trunk to the aorta, bypassing the
pulmonary circulation. Occasionally, the ductus remains patent after birth,
giving rise to serious circulatory abnormalities.
The arterial supply to the heart is
provided by the right and left coronary arteries, which arise from the
ascending aorta just above the aortic valve (Fig. 2.47). They supply the myocardium, including the
papillary muscles and conducting tissue. The principal venous return is via the
coronary sinus and the cardiac veins.
Right coronary artery
This vessel arises from the anterior
aspect of the root of the aorta and descends in the anterior coronary sulcus (Figs
2.47 & 2.48). At the
inferior border, it gives off a marginal branch, which runs to the left towards
the apex of the heart. The right coronary artery continues on the inferior
surface in the coronary sulcus (Fig. 2.49) and terminates by anastomosing with
the circumflex branch of the left coronary artery. On the inferior surface, the
posterior (inferior) interventricular artery arises from the right coronary
artery (occasionally the left coronary artery) and runs in the posterior
interventricular groove towards
the apex. When the
posterior interventricular artery arises from the right coronary artery,
the heart is described as right dominant. The right coronary artery and its
branches supply the anterior surface of the right atrium, the lower part of the
left atrium, most of the right ventricle and parts of the left ventricle and
interventricular septum (Fig. 2.51B). In addition, branches from this artery
usually supply most of the conducting tissue of the heart (p. 56).
This artery takes origin from the
posterior aspect of the root of the ascending aorta and runs to the left behind
the pulmonary trunk where its major branch, the anterior interventricular
artery, arises (Figs 2.47 & 2.50). The latter vessel descends in the
anterior interventricular groove towards the apex of the heart. The left
coronary artery continues as the circumflex artery in the posterior part of the
coronary sulcus and terminates by anastomosing with the right coronary artery.
The vessel supplies the posterior wall of the left atrium and auricle, most of
the left ventricle and parts of the right ventricle and interventricular septum
(Fig. 2.51A).
 |
Fig. 2.50 Left coronary artery and its branches, viewed from the
left.
|
Coronary sinus and cardiac veins
Most of the venous return from the
heart is carried by the coronary sinus, which runs along the posterior part of
the coronary sulcus and terminates in the right atrium. The coronary sinus is
formed near the left border of the heart by the union of the posterior vein
of the left
ventricle and the
great cardiac vein (Fig. 2.52), which accompanies the anterior interventricular
artery. Other veins enter the coronary sinus, including the middle cardiac vein
(Fig. 2.53), which
accompanies the posterior interventricular artery. Some cardiac veins enter the
right atrium independently (Fig. 2.48).
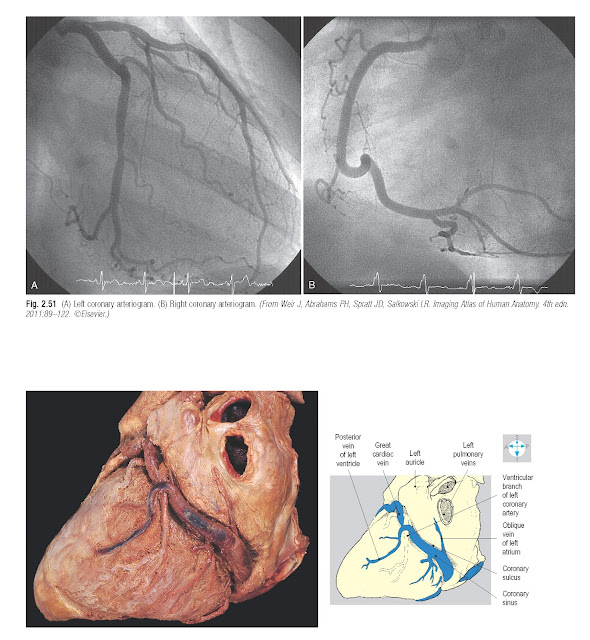 |
Fig. 2.52 Oblique view of the coronary sinus lying in the coronary
sulcus.
|
Conducting
system
Coordinated contraction of the
myocardium is controlled by specialized conducting tissues, consisting of the
sinuatrial (SA) node, the atrioventricular (AV) node, the atrioventricular
bundle (of His) and its right and left branches (Fig. 2.54).
 |
Fig. 2.53 Posteroinferior view of the termination of the coronary
sinus in the right atrium.
|
The SA node lies in the anterior wall
of the right atrium close to the termination of the superior vena cava. It
occupies part of the root of the auricle and the upper end of the sulcus
terminalis. Numerous autonomic nerves supply the node and modify its rate of
discharge. The SA node usually receives blood from an atrial branch of either
the right or left coronary artery. From the SA node the cardiac excitation wave
passes through the atrial myocardium to reach the AV node.
The AV node lies in the interatrial
septum anterosuperior to the termination of the coronary sinus. It is
continuous with the atrioventricular bundle, which passes through the fibrous
ring separating the atria and ventricles. The bundle gains the upper part of
the interventricular septum and promptly divides into right and left branches.
The AV node and bundle are supplied by branches of the posterior
interventricular artery. Interruption of the arterial supply to the conducting
tissues may result in cardiac arrhythmias.
Lying beneath the endocardium, the
right branch of the atrioventricular bundle descends in the interventricular
septum and often passes in the moderator band (Fig. 2.55) to ramify within the anterior wall of the right
ventricle. The left branch runs on the left side of the interventricular
septum. Both branches divide repeatedly at the ventricular apices and spread
out into the myocardium of the respective ventricles.
 |
Fig. 2.54 Location of the conducting tissues.
|
 |
Fig. 2.55 Moderator band, seen through a window cut in the anterior
wall of the right ventricle.
|








