PULMONARY
IMMUNOLOGY LYMPHOCYTES, MAST CELLS, EOSINOPHILS, AND NEUTROPHILS
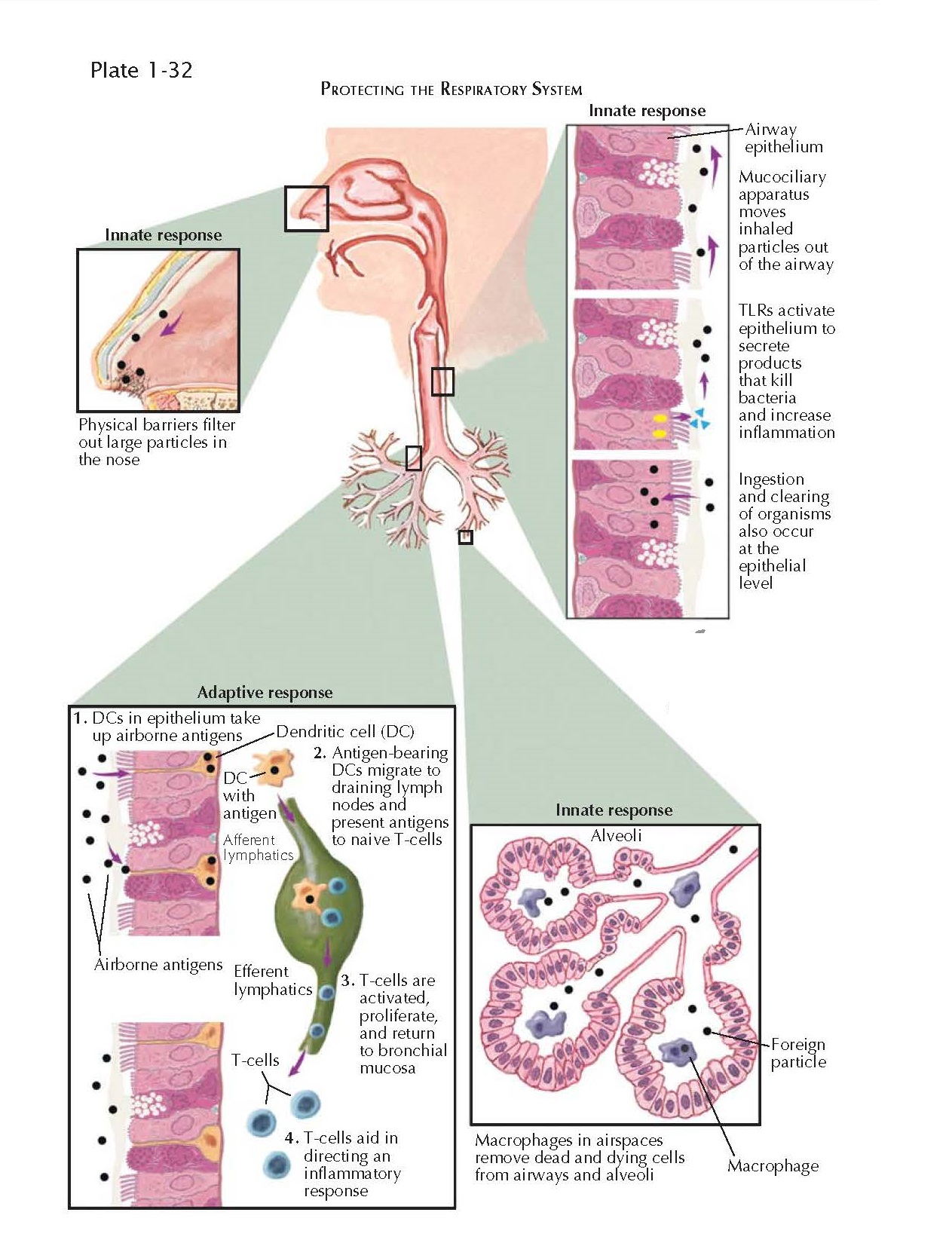
The respiratory system is in
intimate contact with the environment through the inhalation of large volumes
of air every day ( ̴10,000 L). Protecting the respiratory system from pathogens and toxins
while avoiding unnecessary inflammation when harmless proteins are inhaled is a
challenge. Physical barriers such as the filtration of air by the nose and upper
airways and the mucociliary apparatus, which moves inhaled particles,
organisms, and cells toward the pharynx, where they can be swallowed, provide
the first line of defense. Ingestion of organisms and particulate material by
macrophages resident within the lung is another important line of defense.
Ingestion of silica particles or asbestos fibers by macrophages may fail to
clear these particles and may lead to persistence of inflammation and ultimately
lung tissue damage.
The airway epithelial cells
have the capacity to ingest bacteria and have a variety of receptors, such as
Toll like receptors, on their surface that may lead to activation of the
epithelium on exposure to bacterial or viral products (e.g., DNA, RNA,
lipopolysaccharide). Activated epithelium secretes chemoattractant molecules
that will attract neutrophils, eosinophils, and lymphocytes, depending on the
particular need. Cytokines secreted by the epithelium may also promote
inflammation. Defensins are proteins that are secreted by epithelial cells that
may bind to microbial cell membranes and create pores that assist in killing
organisms. Epithelial cells also produce surfactant proteins that may assist in
the elimination of pathogenic organisms.
Adaptive immune responses to
pathogenic organisms and foreign proteins involve lymphocyte populations.
Intraepithelial lymphocytes are usually CD8 + T cells, which are well placed to
exert cytotoxic effects on infected epithelial cells. Indeed, the epithelial
cells are the primary target for a variety of respiratory viruses such as
rhinovirus and adenovirus. After infection, cells may present antigen on their
surface that leads to activation of CD8 + T cells and cell killing through
release of perforin and granzyme or by Fas-Fas ligand interactions. However,
the common cold rhinovirus infects epithelial cells without inducing killing of
these cells and triggers inflammation. Other viruses that target the airway
epithelium such as respiratory syncytial virus (RSV) may cause severe
inflammation of the small airways in infants. Both rhinovirus and RSV are
associated with asthma attacks.
Under the epithelium, there is
a network of dendritic cells. These large cells have projections that protrude
between epithelial cells into the airway lumen and may sample foreign antigenic
substances. After ingestion of foreign protein, these cells migrate to regional
lymph nodes, where they present an antigenic fragment of the protein to CD4+ T
cells with a T-cell receptor with a high affinity for the antigenic peptide. The
subsequent T-cell reaction may lead to the clonal expansion of the cells and
their differentiation into one of several subsets of CD4+ cells. These cells
recirculate and may home to the site of origin of the dendritic cell, where
they may now produce cytokines that play a key role in directing the type of
inflammation. Whereas Th1 type cells are associated with delayed-type
hypersensitivity reactions, Th2 cells may lead to typical eosinophil-rich allergic
inflammation, immunoglobulin E synthesis (IgE), mucous cell differentiation, and
airway hyperresponsiveness. These are all characteristic features of allergic
asthma. Coating of mast cells in the airways, which are recruited after
exposure to aeroallergens, with IgE renders these cells susceptible to
activation by allergens. Release of histamine, growth factors, and cytokines
occurs, and the synthesis de novo of leukotrienes and prostaglandins
contributes to bronchoconstriction and inflammation. Bronchoconstriction is
often biphasic; an early response occurs within minutes and resolves within 1
or 2 hours, and a secondary wave of airway narrowing called the late
response occurs after several hours. This latter reaction is also T-cell
dependent.
Several other T-cell subsets
are of importance in controlling inflammation and host defense. Regulatory T
cells may prevent, limit, or participate in terminating inflammation. Other
newly described T-cell subsets such as Th17 cells are associated with
inflammation that has a strong neutrophilic component, and these cells may be
implicated in more severe forms of asthma. T cells bearing an alternative TCR,
the ᵞᵟTCR, are important in host defense against certain infectious agents,
including Mycobacterium tuberculosis and Pneumocystis jiroveci.
Natural killer (NK) cells and invariant NKT (iNKT) cells participate in
immunologic responses. NK cells are required for protection against several
viral infections, rtussis, and Mycobacterium tuberculosis.