CLINICAL PROBLEMS AND CORRELATIONS
OF SUBAXIAL CERVICAL SPINE
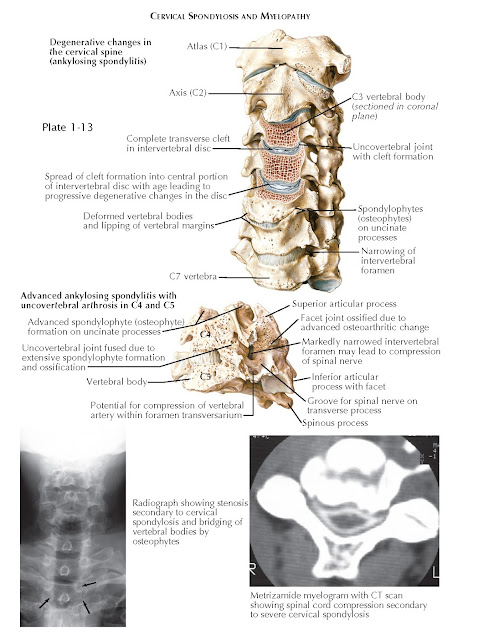
Of all the pathologic processes found in the cervical spine, cervical spondylosis is the most common (see Plates 1-12 and 1-13). It can be found to some extent in all humans as we age. Spondylosis starts with the normal degeneration of the intervertebral disc. As this occurs, the disc progressively loses the ability to maintain its water content. Disc dehydration and other molecular changes to the disc composition result in a decrease in disc height. With loss of disc height, its normal biomechanical characteristics change. As spondylosis progresses, osteophytes form ventrally and posteriorly and the uncovertebral and facet joints hypertrophy. This process occurs to some degree at every spinal functional unit, and it may result in neural compression. It is important to remember, however, that most people remain clinically asymptomatic during this process.
The initial pathologic process in the progression of
cervical spondylosis is intervertebral disc desiccation. As is the case in
other parts of the spine, when the anulus pulposus loses its hydration, the
anulus fibrosis plays a larger role in the weight bearing of the disc. This
results in several pathologic processes, all of which are interconnected.
First, there is an increased frequency of disc herniations into the canal or
foramen. Second, the ventral aspect of the spinal canal must bear an increased
amount of force; and this may lead to loss of cervical lordosis and sometimes
to kyphotic deformity. With continued loss of disc integrity, there is
communication between the dorsal aspects of the vertebral body, which results
in the formation of bone spurs (osteophytes), which then may decrease the space
available for the spinal cord and cause myelopathic symptoms or may extend into
the cervical foramina, causing radiculopathic symptoms (or a combination of the
two myeloradiculopathy).
The pathology of these entities is discussed next.
CERVICAL MYELOPATHY
Cervical myelopathy is a result of encroachment on the
spinal cord (see Plate 1-13). As just described, the process of cervical spondylosis results in a loss of
spinal canal space by several processes. The first is the propensity for
cervical disc herniation, which is caused by disc degeneration but can be
aggravated by thickening, or hypertrophy, of the posterior longitudinal ligament.
The other cause is encroachment by osteophytic processes that result from the
communication of vertebral bodies or uncinate joints that lack cervical disc
buffering. Osteophyte formation is postulated to be a protective mechanism of the spine to increase the surface area of
each vertebral body to better distribute the normal forces of daily activity.
Cervical myelopathy may result from one or both of these processes. It is a
relatively common clinical entity and has significant effects on a patient’s quality
of life. Additionally, preexisting myelopathy can significantly predispose a
patient to serious spinal cord injury after only minor trauma.
Cervical
myelopathy is a constellation of signs and symptoms resulting from spinal cord
dysfunction. Patients with cervical myelopathy present a classic picture of
“upper motor neuron” signs. They have difficulty with gait, balance, and fine
motor coordination in the upper extremities, particularly in movements such as
buttoning a shirt or tying one’s shoes. Weakness and stiffness of the legs is
common, and urinary symptoms of urgency or retention are also possible in later
stages. On examination, patients frequently have hyperactive reflexes below the
level of the spinal cord compression (generally exacerbated in the lower
extremities) and also may demonstrate pathologic Hoffman and Babinski signs.
Motor testing may demonstrate weakness in any of the upper extremity muscle
groups, depending on the severity and level of spinal cord compression. In
advanced disease, the intrinsic muscles of the hand demonstrate impressive
wasting (“myelopathy hand”). Lower extremity strength is variable, with
proximal muscle weakness being more common than distal muscle weakness.
Examination of gait is a valuable clinical tool, because patients with
myelopathy often exhibit a stiff, spastic, or wide-based gait. The clinical
phenomenon of “central cord syndrome” generally occurs when a patient with
preexisting myelopathy sustains a hyperextension injury. These patients present
acutely with upper greater than lower extremity weakness and sensory changes
below the level of their injury. Urinary or fecal incontinence may also be
present. The prognosis for central cord syndrome is favorable.
Observation of these signs and symptoms warrants MRI of the cervical spine and referral to a spine
surgeon. A thorough imaging evaluation with radiographs and MRI provides
adequate assessment of spinal alignment and the location(s), pattern, and
degree of neural compression. Cervical myelopathy is a surgical disease in the
majority of patients because it is usually progressive and, as such, neurologic
deterioration may be permanent. The natural history of cervical myelopathy is
periods of disease stability with intermittent, stepwise decreases in function.
The goal of surgery is to halt disease progression, although some degree of
functional recovery is often observed postoperatively.
CERVICAL RADICULOPATHY
When a cervical nerve root is inflamed or impinged at
the level of the cervical foramen, cervical radiculopathy may occur. It most
commonly occurs as a result of disc herniation in the younger patient or as a
result of nerve root compression due to cervical spondylotic changes.
Compression of the nerve root can result in pain, weakness, or sensory deficits
that correspond to the dermatomal and myotomal distribution of the nerve
itself.
Patients may present with acute or chronic cervical
radiculopathy due to isolated nerve root compression. Patients with existing
cervical myelopathy may also have a radicular pain component, termed cervical
myeloradiculopathy. More than 90% of patients with cervical radiculopathy
improve with nonoperative care. Examination of a patient with cervical
radiculopathy includes a typical motor and sensory examination but also
maneuvers intended to compress the nerve root or to relieve tension on the root
and exacerbate or alleviate symptoms. This may include the shoulder abduction sign, in which the
examiner holds the patient’s hand over the head to alleviate symptoms. The
Spurling maneuver is a provocative test in which the head of the patient is
turned to the side of the symptoms and axial pressure is then applied by the
examiner (see Plate 1-14). This is thought to narrow the intervertebral foramen and exacerbate
the patient’s symptoms. A “positive” Spurling sign is exacerbation of arm pain.
It has been found to be very sensitive, although not specific for
radiculopathy. Observation of the patient in late stages of the disease may
demonstrate wasting of the intrinsic hand muscles if one of the lower cervical
nerves is involved, but, unlike in cervical spondylotic myelopathy, the
findings are unilateral.
Diagnosis of cervical radiculopathy is aided by a
thorough review of plain radiographs (including oblique views), MR images, or a
CT myelogram of the cervical spine. It allows appropriate visualization of the
cervical discs and nerve roots and aids the clinician in preoperative decision
making.
SURGICAL APPROACHES FOR THE TREATMENT OF MYELOPATHY
AND RADICULOPATHY
The decision to employ surgery for cervical myelopathy
or radiculopathy requires a high degree of consideration of its risks,
benefits, and preference of the patient. Surgical treatment of cervical
myelopathy is less controversial given its positive effect on a patient’s
quality of life and the well-known benefits of spinal cord decompression. The
treatment of cervical radiculopathy depends on the etiology (disc herniation or
foraminal narrowing) and on the number of affected nerve roots. Complicating
the surgical approach is that these conditions often occur together, so surgery
may be aimed at alleviating both myelopathy and radiculopathy in a single
operation. An important distinction to remember between radiculopathy and
myelopathy is the former is typically a nonoperative disease whereas the latter
is a surgical one. That is, a radiculopathy usually responds very favorably to
nonoperative care.
Anterior Approach to the Cervical Spine
One of the most common spine surgeries performed is the
anterior cervical discectomy and fusion. Patients who have degenerative changes
of the spine involving mainly the ventral aspect of the spinal cord or nerve
root(s) are likely to benefit from this procedure. The surgery involves an
incision just lateral to the midline of the neck, and a dissection lateral to
the trachea and medial to the carotid sheath of the neck to approach the anterior cervical spine. From there, the prevertebral
fascia is incised and the intervertebral disc is exposed and removed, as is the
posterior longitudinal ligament. This exposes the ventral dura and exiting
roots. This may be performed at one or multiple levels in the spine. An
intervertebral graft (tricortical iliac crest autograft, cadaveric allograft,
or synthetic cage) is used to replace the intervertebral disc to facilitate
fusion of the adjacent vertebrae. The addition of an anterior cervical plate improves fusion rates and prevents graft dislodgment. Another option for
ventral treatment of both radiculopathy and myelopathy is cervical disc
replacement, which utilizes the same approach to the spinal column. Cervical
corpectomy (removal of the central vertebral body) is indicated for spinal cord
compression occurring behind the vertebral body or in cases of osteomyelitis or
tumor.
Posterior Approaches to the Cervical Spine
For select patients with myelopathy or
myeloradiculopathy, decompressive posterior surgery may be appropriate. Two
common procedures are laminectomy with instrumented fusion and laminoplasty of
the cervical spine. In both procedures, a midline incision is made in the neck
and the overlying muscles are dissected from bone to expose the spinous
processes and laminae. The laminae and spinous processes are either removed
(laminectomy) or are altered to expand the cervical spinal canal
(laminoplasty). There are multiple laminoplasty techniques.
Radiculopathy can be often treated posteriorly via a
decompression of the foramen and lamina (laminoforaminotomy). These procedures
are typically attempted at one or two levels, are performed unilaterally, and
may offer significant symptomatic improvement to the appropriately selected
patient.
VERTEBRAL ARTERY DISSECTION
Like all arteries, the vertebral artery consists of an
intima, media, and adventitia. Whereas the term dissection is often
applied to any vertebral artery injury, there exists a gradient of damage that
is observed. A small intimal tear, for example, may have minimal, if any,
clinical consequences. A true dissection of the vertebral artery refers to the
creation of a tear through the intima allowing blood to enter into the arterial
wall. The arterial pulsations result in a growing amount of blood in the
arterial wall and lead to thrombosis. If blood ruptures through the wall
entirely, a hematoma is created. This is known as a pseudoaneurysm, which may
also be catastrophic if the lumen becomes occluded. The furthest end of the
spectrum is vertebral artery transection, which is frequently fatal regardless of which vertebral artery is
affected.
The vertebral artery is well protected by the transverse foramina between C6 and C1. This bony protection comes at a cost: whereas
the bony ring of the transverse foramen prevents injury of the artery during
low-energy trauma, fracture of the transverse foramen from a high-energy
mechanism places the vertebral artery at risk of injury from bony impingement.
The majority of patients
found to have a vertebral artery dissection after blunt trauma have associated
cervical spine trauma. Nontraumatic dissections are often spontaneous.
Much attention is paid to rare, but nonetheless
important, causes of vertebral artery injury. These include chiropractic
manipulation, contact sports, and yoga. There are several anatomic
considerations that make these events more likely to occur. First, the vertebral
artery is relatively susceptible to different forces at two points during its
course. The first is between the atlas and the axis, where high rotary
potential allows for the possibility that a forced, high-energy, high-velocity
rotation may cause damage. This is what may occur during certain chiropractic
manipulations. The other site is at the extraosseous (V3) segment where the
vertebral artery lies in the sulcus arteriosus prior to piercing the dura on
its course to the brain. At this level, the vertebral artery is truly
unprotected by major bony landmarks, and activities causing prolonged
hyperextension may result in vertebral artery damage. The effects of vertebral
artery dissection are related to the neurologic structures that it sustains,
and damage can occur via several mechanisms. Dissection or embolism can cause
occlusion or diminished flow to the posterior circulation, creating
vertebrobasilar insufficiency. Clinically, dizziness, ataxia, altered level of
conscious- ness, and visual changes may be observed. Rarely, blood supply to
the anterior spinal cord may be compromised if the anterior spinal artery
(which arises from the vertebral artery) is affected. If the damaged vertebral
artery is anomalous and feeds the posterior inferior cerebellar artery without
joining to form the basilar artery, then lateral medullary syndrome (Wallenberg
syndrome) can result. A constellation of symptoms results, including an
ipsilateral Horner syndrome, facial numbness, and cerebellar deficits, as well
as contralateral numbness below the neck.
If a vertebral artery dissection is suspected, the
gold standard diagnostic tool is the angiogram. If angiography is unavailable
or not clinically advisable, a CT- angiogram may be obtained. The treatment of
a dissection ranges from medical treatment alone with anticoagulation and blood
pressure support to endovascular stenting or surgical intervention depending on
the type and severity of the pathologic process.
LOCKED FACETS
Locked facets (also known as “jumped facets”) are the
result of spinal trauma and can occur unilaterally or bilaterally. The
consequences of this distinction are significant because the resultant
differences in treatment and outcomes diverge greatly. Bilateral locked facets
are the result of
traumatic hyperflexion injuries, and a majority of those patients presenting
with bilateral locked facets are quadriplegic. Those with incomplete spinal
cord injury have some potential for recovery, but the prognosis remains poor.
There exists debate as to whether reduction should be undertaken closed (with
traction) or open (using pins to distract the spine intraoperatively before
surgical fixation). Unilateral locked facets are also the result of hyperflexion, but a component of rotational
subluxation is implied (the rotation is thought to cause only a single locked
facet). These patients tend to present with less severe findings of a
neurologic examination and may be neurologically intact. Depending on the
concurrent fractures present in the spine, these patients may ndergo closed
reduction with a high rate of success.