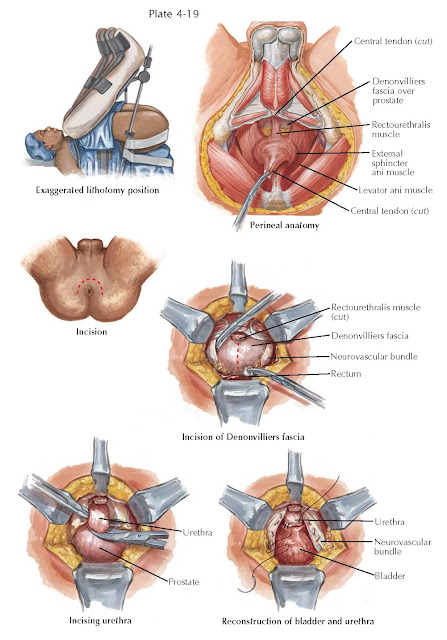
MALIGNANT PROSTATE SURGERY I PERINEAL
The radical perineal prostatectomy was first described as a surgical cure for prostate cancer in 1905. Its popularity waned in the late 1970s as the importance of the pelvic lymph node dissection for accurate staging was elucidated. More recently, there has been renewed interest in this anatomic approach to prostate cancer as more accurate staging methods have reduced the need for staging lymph node dissection. In addition, similar to its advantages in benign prostate surgery (see Plate 4-16), the perineal approach for prostate cancer treatment offers unmatched visualization of the apical prostate and urethral dissection, is important for cancer cure, and is associated with less blood loss. Unlike with the retropubic approach, a full bowel preparation is given the day before perineal surgery. After the induction of anesthesia, the patient is placed in an exaggerated lithotomy position; severe hip ankylosis or unstable prosthetic hips may thus be a contraindication to this approach. A curved Lowsley retractor is placed transurethrally into the bladder and its wings opened. A curvilinear incision is made around the anus as described for the perineal prostatectomy for benign prostatic hyperplasia (BPH; see Plate 4-16). After bluntly developing the ischiorectal fossa on each side, the central tendon is cut and the longitudinal muscle fibers of the rectum identified. With gentle traction on the rectum, dissection is carried superiorly until the rectourethralis muscle, which connects the rectum to the perineal body, is identified. The rectourethralis muscle is divided close to the prostatic apex, allowing the rectum to fall dorsally. The risk of rectal injury is highest at this point. Ideally, this dissection is between the leaves of Denon-villiers fascia. With pressure on the Lowsley retractor, the prostate is delivered into the field, allowing blunt, digital dissection of the prostate until its base is identified at the vesicoprostatic junction.
Unlike with perineal prostatectomy for BPH, the prostatic capsule is not
incised when the entire gland is to be removed. Instead, the exposed
anterior layer of Denon villiers fascia is incised
vertically in the midline from the base to the apex of the prostate to preserve
the neurovascular bundles. Careful lateral dissection and gentle traction help
to preserve the neurovascular bundles as they course between the leaves of
Denonvilliers fascia. At the prostatic apex, the bundles are also dissected
free of the urethra, and the posterior urethra is incised sharply over the
Lowsley retractor. With traction on the retractor, the anterior urethra is then
transected and the prostate freed to the bladder neck by sharp and blunt
dissection. The puboprostatic ligaments are then transected. Care is needed to
avoid injuring the dorsal venous complex during this dissection of the anterior
prostate.
The prostate bladder neck junction is identified by palpation of the wings
of the Lowsley retractor. With sharp and blunt dissection, the bladder neck is
preserved. The bladder neck is first incised anteriorly to avoid injury to the
ureteral orifices posteriorly. With traction on the prostate, the bladder neck
incision is continued circumferentially around the prostate base, dissecting
and ligating the lateral pedicles coursing toward the prostate. Ligation of
these pedicles is performed close to the prostate to avoid injury to the
adjacent neurovascular bundles. With further posterior dissection, the paired
vasa deferentia are ligated and transected and the seminal vesicles are excised
with the prostate.
After the specimen is removed, the bladder neck is easily visible.
Occasionally, it may be necessary to reconstruct the
bladder neck in a “tennis racket” fashion with absorbable suture. Accurate
anastomotic suture placement between the bladder neck and membranous urethra is
guided by better visualization of these structures with the perineal method
compared to the retro- pubic approach. A Penrose drain is placed near the
bladder neck anastomosis and brought out through the skin incision. The levatorani muscles and central tendon are then reapproximated, and the skin closed
with interrupted vertical mattress sutures. Patients are advised to ambulate the evening of surgery, and the drain is removed and
patients are advanced to a regular diet the day after surgery. Rectal
stimulation and medications are prohibited. Hospital discharge is on day 1 or 2
after surgery. Unique but infrequent complications of the perineal
prostatectomy are transient lower extremity sensory neurapraxia (2%), and
rectal incontinence (3%). Rates of urinary incontinence and erectile
dysfunction are comparable to those of retropubic
methods.