Structure of Small Intestine
 |
| MUCOSA AND MUSCULATURE OF DUODENUM |
The freely mobile portion of the small intestine, which is attached to the mesentery, extends from the duodenojejunal flexure to the ileocolic orifice, where the small intestine joins the large intestine. This portion of the small intestine consists of the jejunum and the ileum. They run imperceptibly into each other, the transition being marked by a gradual change in the diameter of the lumen and by several structural alterations.
The
walls of the jejunum and ileum are virtually identical in structure but have
slight modifications that make them histologically distinct. Like the rest of
the gastrointestinal tract, the jejunum and the ileum each has four layers: the
mucosa, submucosa, muscularis externa, and serosa. The innermost
layer, the mucosa, is thickly plicated by macroscopically visible circular
folds (plicae circulares, Kerckring folds). These folds vary in height,
projecting into the lumen by 3 to 10 mm. Some of these plicae extend all the
way around the internal circumference, some of them extend only halfway or two
thirds of the way around the circle, and still others spiral around the circle
twice or even more times. The circular folds projecting into the lumen slow
down the progression of the luminal contents to a slight degree, but their most
important function is to increase the absorptive surface area of the intestinal
lumen. The visible increase in surface area created by the circular folds is
mirrored on the microscopic level by tiny fingerlike projections, intestinal
villi.
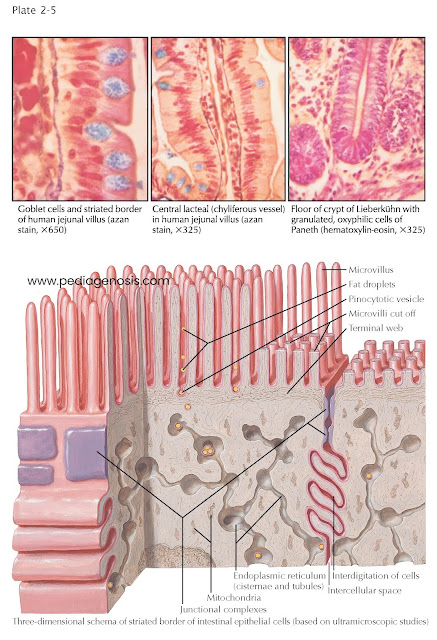
In
fact, the entire mucosal surface of the small intestine, over and between the
circular folds, is covered with intestinal villi, projections that are 0.5 to
1.5 mm long (just barely visible to the naked eye). The mass of these villi
(estimated at 4 million altogether in the jejunum and ileum) accounts for the
velvety appearance of the mucosa. They are somewhat longer and broader in the
jejunum than they are in the ileum. The valleys or indentations between the
villi form nonramified pits, each of which harbors tubular structures, the intestinal
glands (crypts of Lieberkühn). Along the villi, the entire inner surface of
the small intestine is covered by a single layer of epithelial cells, the
majority of which are enterocytes, highly prismatic columnar cells with
a surface covered by microvilli, microscopic projections from these
cells’ apical surfaces. Between these columnar cells are interspersed three
other types of cells: goblet cells, Paneth cells, and enteroendocrine
cells. The goblet cells secrete an alkaline, mucous fluid that coats the
whole mucosa. Most goblet cells are found lining the crypts or along the lower
parts of the villi, but a considerable number of them are located near the apex
of the villi, where they seem to be squeezed between neighboring enterocytes.
The Paneth cells are found almost exclusively near the base of the glands. They
are easily identified histologically due to the eosinophilic granules they
contain. Paneth cells are primarily involved in moderating the bacterial normal
flora of the small intestine. They do so by
secreting the antimicrobial enzyme lysozyme, as well as α-defensins. They are able
to phagocytose bacteria and other invaders within the intestinal lumen. Lastly,
the enteroendocrine cells (argentaffin cells, yellow cells, cells of Schmidt or
of Kultschitzky) contain basal-staining granules with a high affinity for
silver and chromium. These cells are typically found at the bottom of
intestinal glands but can migrate upward. They regulate the activity of the digestive
system by releasing hormones such as cholecystokinin (stimulates secretion of
the gallbladder and pancreas and inhibits gastric emptying), secretin
(stimulates pancreatic secretion and inhibits gastric secretion), motilin
(stimulates peristalsis), and gastric inhibitory peptide (stimulates insulin
secretion and inhibits gastric secretion) into the bloodstream. Enteroendocrine
cells in the small intestine may also secrete somatostatin (inhibits release of
gastrin and gastric secretion) and histamine
(stimulates gastric secretion from parietal cells) in a paracrine fashion,
affecting nearby tissues. Lymphocytes, eosinophils, neutrophils, macrophages,
mast cells, and plasma cells are also sometimes seen in the epithelial lining
of the small intestine, but these have generally migrated from the underlying
layer of the mucosa, the lamina propria.
The
lamina propria lies deep to the epithelial surface of the mucosa, but it
extends into both the circular folds and intestinal
villi, forming the core of each villus. This diffuse reticular connective
tissue allows for the easy diffusion of nutrients and gasses to and from the epithelial
lining of the intestine. The lamina propria frequently assumes a lymphatic
character owing to the large number of lymphocytes that migrate through it. The
lamina propria also contains thin fibers of smooth muscle that radiate from the
muscularis mucosae and extend upward to the tips of the villi. When these
fibers are relaxed, the villi have a smooth surface, whereas they become jagged
or indented when the fibers contract. These muscular fibrils are assumed to act
as motors that maintain the pumping function of the villi. At the core of each
villus is a lymphatic vessel, the central lacteal, which transports
fat-soluble substances and lymph to the cisterna chyli and from there to the
venous circulation. The muscularis mucosae, which separates the lamina
propria from the submucosa, is com- posed of two thin layers of smooth muscle,
which keep the movable mucosal layer in place. The outer longitudinal layer is
thinner than the inner circular layer, from which the muscular fibers in the
core of the villi, mentioned above, emanate.
 |
| SMALL INTESTINE MICROSCOPIC STRUCTURE |
The
submucosa is a relatively stout layer that is located deep to the
mucosa. It is made up of type I collagen bundles forming dense, irregular
connective tissue. By altering the angles of its meshes, this submucosal
network is able to adapt itself to changes in the diameter and length of the
intestinal lumen. The submucosa contains a rich network of arteries, veins, and
lymphatics that supply the submucosa and overlying mucosal structures. It also
has a substantial network of viscerosensory and visceromotor axons;
preganglionic parasympathetic axons terminating in the submucosa synapse on the
submucosal plexus (Meissner plexus), a collection of ganglia (nerve
cells) scattered throughout the small and large intestines that contribute to
the enteric nervous system. The muscularis externa is a large and
powerful two-layered coat of smooth muscle that covers the submucosa. The thick
inner circular layer and the thinner outer longitudinal layer are connected by
convoluted transitional fascicles in the area where they border on each other.
Between the two layers is a network of viscerosensory and visceromotor axons.
As in the sub-mucosa, preganglionic parasympathetic axons synapse with the myenteric
plexus (Auerbach plexus), which are the ganglia located between the two
layers of smooth muscle. The myenteric plexus and submucosal plexuses are major
components of the enteric nervous system. The muscularis externa is responsible
for creating the powerful movements of peristalsis that move intestinal
contents progressively down the lumen, or in retrograde motion during vomiting.
Lining
the outside surface of the small intestines is the final layer, the serosa (visceral
peritoneum). This layer is composed of mesothelial cells on the surface that
are connected to the muscularis externa by a thin layer of loose connective
tissue. The mesothelial cells release fluid that lubricates the external
surface of the small intestine and helps to prevent irritation and adhesions between
the intestines and other peritoneal structures. The serosa covers the entire
circumference of the small intestines, except for a narrow strip where the
mesentery anchors the intestines to the posterior body wall.
Though
very similar in many ways, the jejunum and ileum differ in several respects.
The lumen of the ileum is narrower and the diameter of the total wall is
thinner than that of the jejunum. The average diameter of the jejunum measures
3 to 3.5 cm and that of the ileum 2.5 cm or
less. Due to this difference, the contents of the intestine are more visible
through the wall of the ileum than the jejunum. Because of this, in the operative
view, the jejunum typically has a whitish-red hue, whereas
the ileum takes on a darker appearance. The circular folds within the lumen
vary in frequency and height, as do the villi. They decrease in height and
number as the small intestine approaches the cecum, and in the distal ileum the
folds appear only sporadically.
In
the jejunum, lymphatic tissue is encountered only in the form of solitary
lymphoid nodules that appear as pinhead-sized elevations on the surface of
the mucosa.
They
become more numerous and more pronounced as they near the large intestine.
However, within the ileum, such nodules are very pronounced, forming aggregated
lymphoid nodules (Peyer patches). They are invariably situated opposite the
attachment of the mesentery and are generally of an elongated oval or ellipsoid
shape, their longest diameter always coinciding with the longitudinal axis of
the intestinal lumen. Their average width is 1 to 1.5 cm and they vary in
length from 2 cm up to 10 or 12 cm or, occasionally, even more. They differ in
number from one individual to another, the average total fluctuating from 20 to
30. Another difference between the jejunum and ileum concerns the fat content
of their mesenteries. In the adult, the mesentery of the ileum contains more
fatty tissue and appears to be thicker than that of the jejunum. The blood
vessels that supply each region also have a different appearance, which is
described in Plates 1-1 and 1-2.
The
principal task of the gastrointestinal tract is to supply the body with its
caloric requirements and metabolic material. The structures of the entire gastrointestinal
tract, from the mouth to the large intestine, are optimized to accomplish this
task. It is within the small intestines, especially the jejunum and ileum,
where the majority of absorption occurs through the long row of epithelial
cells, enterocytes, which coat the inner surface of the small intestine. These
epithelial cells, together with the villi they cover, should properly be
considered the organ of absorption. The surface area available for
absorption is maximized in several ways. The circular folds of the small
intestine (including the epithelial cells, lamina propria, muscularis mucosae,
and submucosal layers) increase the surface area grossly. The villi that
project from the lumen and circular folds further increase the surface area
available for absorption. Finally, the apical surfaces of the enterocytes
themselves have a striated border, which is actually composed of microvilli
extending from each enterocyte into the lumen. It has been calculated that each
epithelial cell is provided with about 1000 microvilli, which increase the
cellular surface approximately 24 times. The microvilli seem to vary only a
little in size (average length, 1 micron; width, 0.07 micron) and have a core
of actin microfilaments extending down their length to attach to a network of
fibrils, the terminal web, at the apical edges of the cells. Contraction
or relaxation of this web can widen or narrow the space between adjacent villi.
At
some time after the ingestion of a meal containing fat, fine lipid droplets can
be observed in the intermicrovillous spaces; slightly later, the droplets
appear in the area of the terminal web, where they accumulate in minute
vesicles, which owe their existence to a pinocytotic activity, probably
of the intermicrovillous plasma membrane. The droplets then can be found in the
main body of the epithelial cell, where they coalesce to form larger units in
vesicles or cisternae, which are connected with each other by intracellular
tubules. The fat drop- lets pass toward the lateral cell surfaces. From the
inter- cellular spaces, the droplets traverse the basement membrane and the
interstitial spaces of the lamina propria to enter the central lacteals of the
villi. The lacteals carry fats and fluid
proximally via lymphatic channels that ultimately drain to the cisterna chyli,
thoracic duct, and, finally, left subclavian vein. For this reason, fat-soluble
substances can bypass the liver, which receives the substances from the lumen
that are transported to it via the hepatic portal vein.
 |
| EPITHELIUM OF SMALL INTESTINE |
The nucleus of the enterocytes is typically located in its basal region, near the Golgi apparatus. Mitochondria and other organelles of the cell body show no particular or specific features. To maintain a separation between the lumen of the intestines (which is technically outside the body) and the extracellular space within the body, the apical region of enterocytes and other cells of the intestinal epithelium are bound to each other by junctional complexes in the vicinity of the terminal web. The enterocytes are anchored to the underlying connective tissue of the lamina propria by tight junctions. This allows the enterocytes to be selective about the substances that are released into the lamina propria and, thereafter, the bloodstream.




