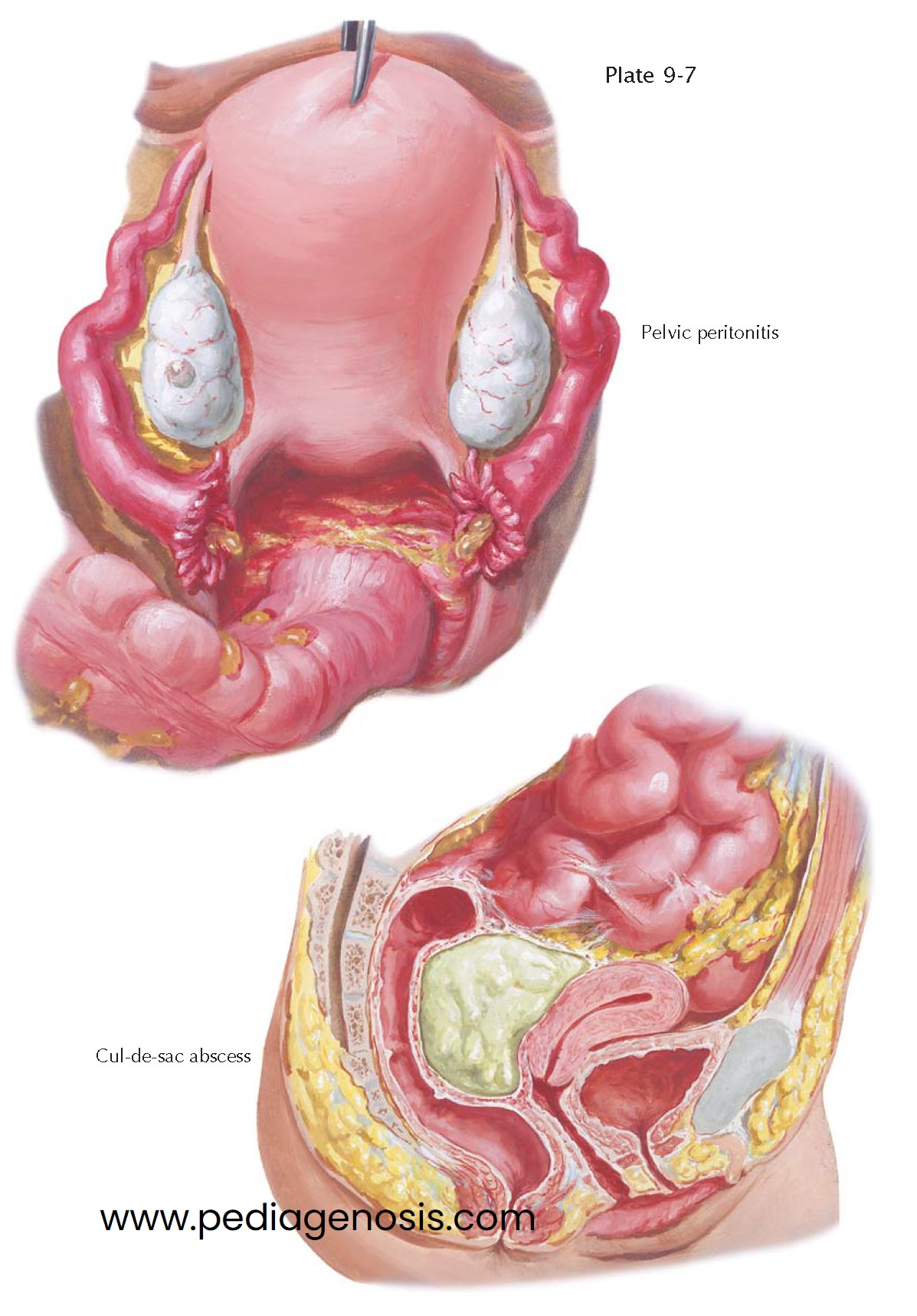
PELVIC PERITONITIS, ABSCESS
As long as the ampullary ostium is patent, the purulent contents of the infected tube escape into the peritoneal cavity, causing a peritonitis, which is at first diffuse but, in favorable cases, may become confined to the pelvic cavity. Even when the tubes have become blocked, widespread peritonitis may result from spread of perisalpingitis, tubal lymphangitis, or rupture of a tube. Whereas acute parametritis often leads to septicemia, if the loose or liquefied infected thrombi enter the general circulation, acute salpingitis causes a diffuse or circumscribed pelvic peritonitis. Thus, pelvic inflammatory disease (PID) is a serious, diffuse, frequently multiorganism infection of the pelvic organs that results in significant morbidity.
The severity and extent of the peritonitis depend on the type of pathogenic
bacteria, their virulence, the resistance of the patient, and the efficiency of treatment.
In roughly one-third of cases, the causative organism is Neisseria gonorrhoeae
alone. One-third of cases involve infection with N. gonorrhoeae and additional
“mixed” infections with other organisms. The last third of infections are due to
mixed aerobic and anaerobic bacteria, including respiratory pathogens such as Haemophilus
influenzae, Streptococcus pneumoniae, and Streptococcus pyogenes found
in up to 5% of patients. Polymicrobial infections are present in more than 40%
of patients with laparoscopically proven salpingitis, with one study reporting an
average of 6.8 bacterial types per patient. Only approximately 15% of women
with cervical N. gonorrhoeae infections develop acute pelvic infections.
Orgasmic uterine contractions, disruption of normally protective cervical mucus
at ovulation or during menses, the attachment of N. gonorrhoeae to sperm
or direct inoculation at the time of surgical procedures, like placement of an intrauterine
device (IUD), may provide transportation to the upper genital tract. Chlamydia
is involved in roughly 20% of patients, with this rate rising to roughly 40%
among hospitalized patients. Infection of the upper genital tract by Chlamydia
often causes an indolent course of salpingitis with more insidious symptoms.
During upper genital tract infections, purulent material accumulates in the
cul-de-sac and may become sealed off from the rest of the peritoneal cavity by adhesions
between the pelvic organs, omentum, and intestinal loops. Frequently, the sigmoid
and the mesosigmoid become adherent to the uterine fundus and the upper border of
the broad ligament, forming a protective roof over the pocket of pus. This pelvioperitonitic
abscess, commonly called a tuboovarian abscess, is a protective mechanism to localize
and contain the infectious process.
A tuboovarian abscess can be surgically opened and drained via the anterior
abdominal wall, by laparotomy or laparoscopy, or by a transvaginal route. In some
unique situations, interventional radiologists may drain a tuboovarian abscess by
inserting an imaging guided catheter into the affected area. Pelvic peritonitis
very seldom heals without leaving adhesions between the pelvic organs, the sigmoid,
and the omentum. Very often, the uterus is pulled backward into a permanent
state of retroflexion by adhesions with the rectum and the pelvic wall. This fixed
uterine retroflexion can cause troublesome symptoms such as backache, constipation,
and pain during defecation and copulation. Surgical extirpation may be the only
option when symptoms are significant and unresponsive to other therapies.
Roughly one in four women with acute PID experiences medical sequelae. Pelvic inflammatory disease leads to tubal factor infertility, ectopic pregnancy, and chronic abdominal pain in a high percentage of patients. The risk of infertility roughly doubles with each subsequent episode, resulting in a 40% rate of infertility after only three episodes. One single episode of severe PID can cause infertility. Women with documented salpingitis have a fourfold increase in their rate of ectopic pregnancy, and 5% to 15% of women require surgery because of damage caused by pelvic inflammatory disease. Peritoneal involvement may spread to include perihepatitis (Fitz-Hugh-Curtis syndrome). Rupture of a tuboovarian abscess, with subsequent septic shock, may be life-threatening.