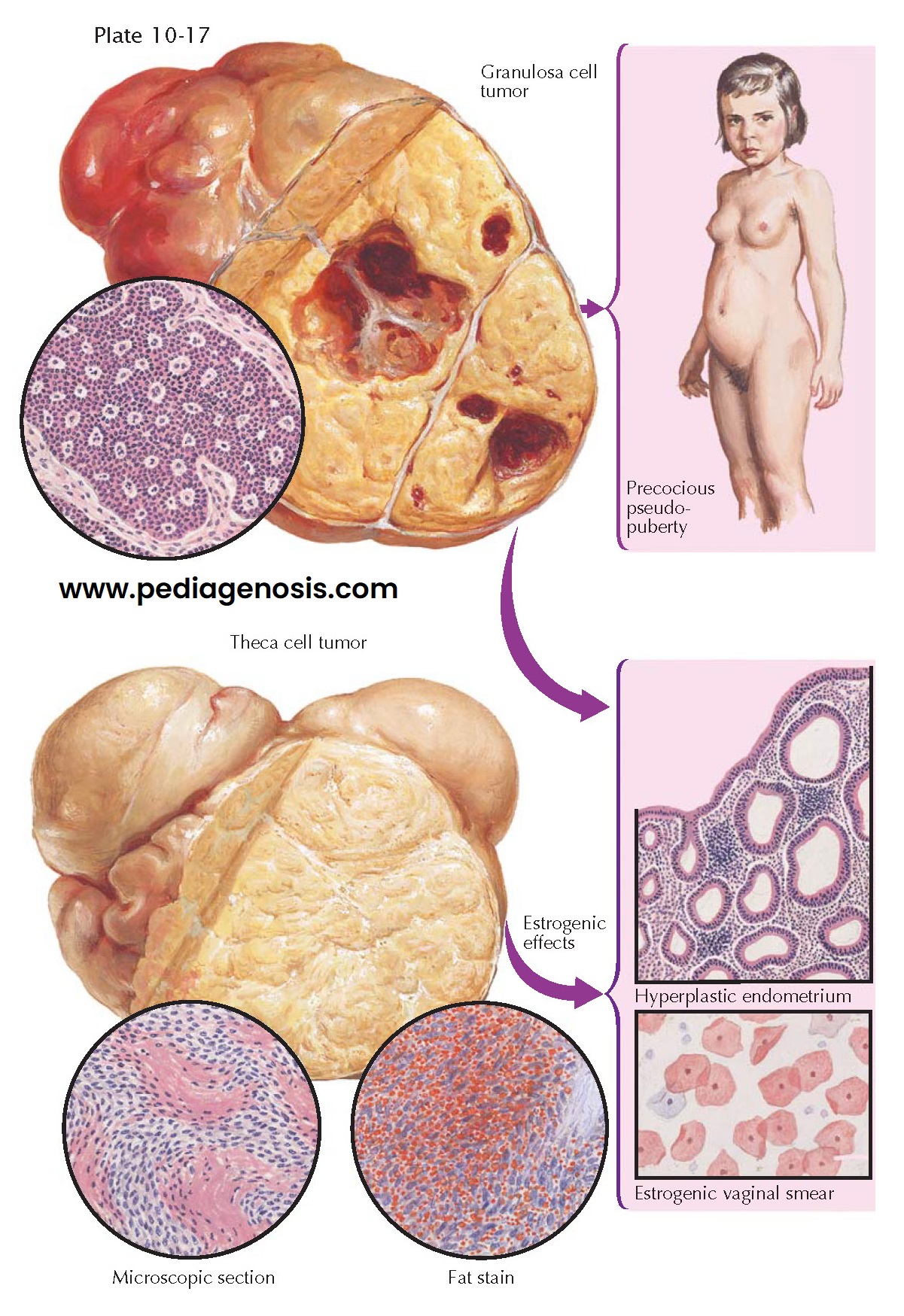
FEMINIZING NEOPLASMS
The granulosa cell tumor is a feminizing neoplasm composed of cells that resemble, in appearance and arrangement, the granulosa cells of the graafian follicle. It is the most common of the hormonal tumors of the ovary, comprising 6% of all ovarian tumors. Unlike theca cell tumors, it may be found in the prepubertal years (5%). The degree of hormonal activity is variable. The clinical characteristics depend upon age: in child-hood, hyperestrogenism is responsible for the syndrome of precocious pseudopuberty manifested by the premature development of secondary sex characteristics (feminine contour, breast growth, pubic and axillary hair, enlargement of the genitalia, anovulatory menses, acyclic uterine bleeding, hyperplastic endometrium, and estrogenic vaginal smears); during sexual maturity, the granulosa cell tumor may induce irregular vaginal bleeding; postmenopausally, irregular uterine bleeding, a marked estrogenic vaginal smear, and endometrial proliferation or hyperplasia. Breast enlargement, uterine fibroids, endometrial hyperplasia with polyps, and a concomitant endometrial carcinoma may develop. The tumor, by virtue of its size and weight, may give rise to abdominal pain, pressure symptoms, and torsion of the pedicle with infarction, hemorrhage, rupture, ascites (10%), and Meigs syndrome. Prognosis does not correlate with the histologic pattern of the tumor: 90% of tumors found are stage I and the prog- nosis is good (90% 10-year survival); a poorer prognosis is found with tumors 15 cm that have ruptured or have a high mitotic rate or aneuploidy.
Granulosa cell tumors are usually unilateral (98%), solid, movable, round
to oval, encapsulated neoplasms, with a smooth, lobulated, yellow-tan surface.
Their consistency is moderately firm or soft, depending upon the degree of
necrosis and cystic degeneration. They vary in size from a few millimeters to
40 cm in diameter. Section reveals solid or partially cystic, cellular,
granular, slightly trabeculoid tumors, with large areas of grayish-white to
yellow or tan-brown color, scattered necrotic foci, hemorrhage, and
liquefaction.
Derived from the sex cords of the ovary and the stroma of the developing
gonad, these tumors have a predominance of granulosa cells. Classically, these
tumors contain eosinophilic bodies surrounded by granulosa cells (Call-Exner
bodies). Poorly differentiated tumors may be confused with adenocarcinomas
(especially small cell carcinoma).
Theca cell tumors are benign, unilateral, solid, estrogen-producing
neoplasms composed of cells resembling the theca interna. They are
histogenetically and biologically similar to the granulosa cell tumors, which
may coexist to a greater or lesser degree. The majority occur during the
menopausal and postmenopausal years (70%), are rarely seen before 30 years of
age, and do not occur before puberty. Their hormonal effects are similar to
those of the granulosa cell neoplasms.
Theca cell tumors are solid, round to oval, slightly irregular, firm,
encapsulated, yellowish and fibromatous, varying from a few millimeters to 22 cm
or more in diameter. The surface is smooth, free of adhesions, and grayish
yellow. On section, interlacing strands and whorls of tissue suggest a
fibroma-like appearance. The essential difference from the granulosa cell tumor,
however, is the presence of areas of yellowish hue, which may, at times, be
more orange, tan, or brown. Foci of necrosis, cystic degeneration, and
calcification may occur.
Histologically, the tumor is composed of interlacing, broad sheets of cells, showing varying degrees of cellularity. Bands of collagenous, fibrous tissue may separate bundles of typical thecoma cells. The characteristic theca cells have an epithelioid appearance, are elongated and ovoid, with plump, oval nuclei, indistinct borders, and moderate fibrillar, reticulated, and occasionally vacuolated cytoplasm. Clusters of more spherical, luteinized cells may also be seen. Hyaline plaques and collagenous strands are irregularly distributed throughout the tumor. The ovarian parenchyma in the involved and uninvolved ovaries may show evidences of stromal hyperplasia and thecomatosis.