Delirium
and Acute Personality Changes
Delirium is an acute confusional state commonly
seen in patients with medical illness, especially among the geriatric
population. Delirium encompasses four key clinical features, including (1) a
disturbance of consciousness with impaired attention and concentration, (2) the disturbance develops over
a short period of time (hours to days) and often fluctuates in
severity. (3) a perceptual disturbance that is not related to a
pre-existing condition such as dementia, and (4) an underlying medical
condition, intoxication, or medication side effect is evident.
Approximately 30% of older patients experience delirium in the course of
hospitalization, with higher rates among more frail patients and those
under-going complex surgery. In the intensive care unit (ICU), the prevalence
of delirium is about 70% as measured by standardized screening and diagnostic
tools.
There are multiple pathophysiologic mechanisms that may cause delirium; there is no final common pathway allowing a simple approach to diagnosis or treatment. The neurobiologic basis of delirium is, therefore, poorly understood, and diagnosis relies on a comprehensive clinical assessment with judicious use of ancillary studies. In general, areas of the brain that govern arousal, attention, insight, and judgment are affected. These include the subcortical ascending reticular activating system (ARAS) and integrated cortical regions. The ARAS predominantly serves arousal mechanisms, whereas integrated cortical function is necessary for proper orientation to person, place, and time, as well as higher cognitive functions.
Of the neurochemical
pathogenic mechanisms of delirium, the best understood is the cholinergic
system. Anticholinergic drugs are commonly associated with delirium in healthy
patients but much more so in the elderly. Conditions that may predispose to
delirium secondary to acetylcholine depletion include hypoxia, hypoglycemia,
thiamine deficiency, and Alzheimer disease. In addition, many commonly used
drugs may precipitate delirium due to secondary anticholinergic effects.
Additional neurotransmitter systems that may precipitate delirium include GABA,
endorphins, neuro-peptides, serotonin, and norepinephrine. Other neuro-chemical
precipitants of delirium include endogenous chemicals, such as proinflammatory
cytokines and tumor necrosis factor-alpha, which may explain delirium occurring
in the context of infection/sepsis, surgery, and hip fractures. The
blood-brain barrier is weakened by sepsis, even in pediatric cases. Other
than advanced age, pre-existing CNS disease, such as Alzheimer disease,
Parkinson disease, stroke, etc., accounts for a significant increase in risk
for delirium. Indeed, a new delirium in an elder patient may be a heralding
sign of previously unrecognized or impending dementia.
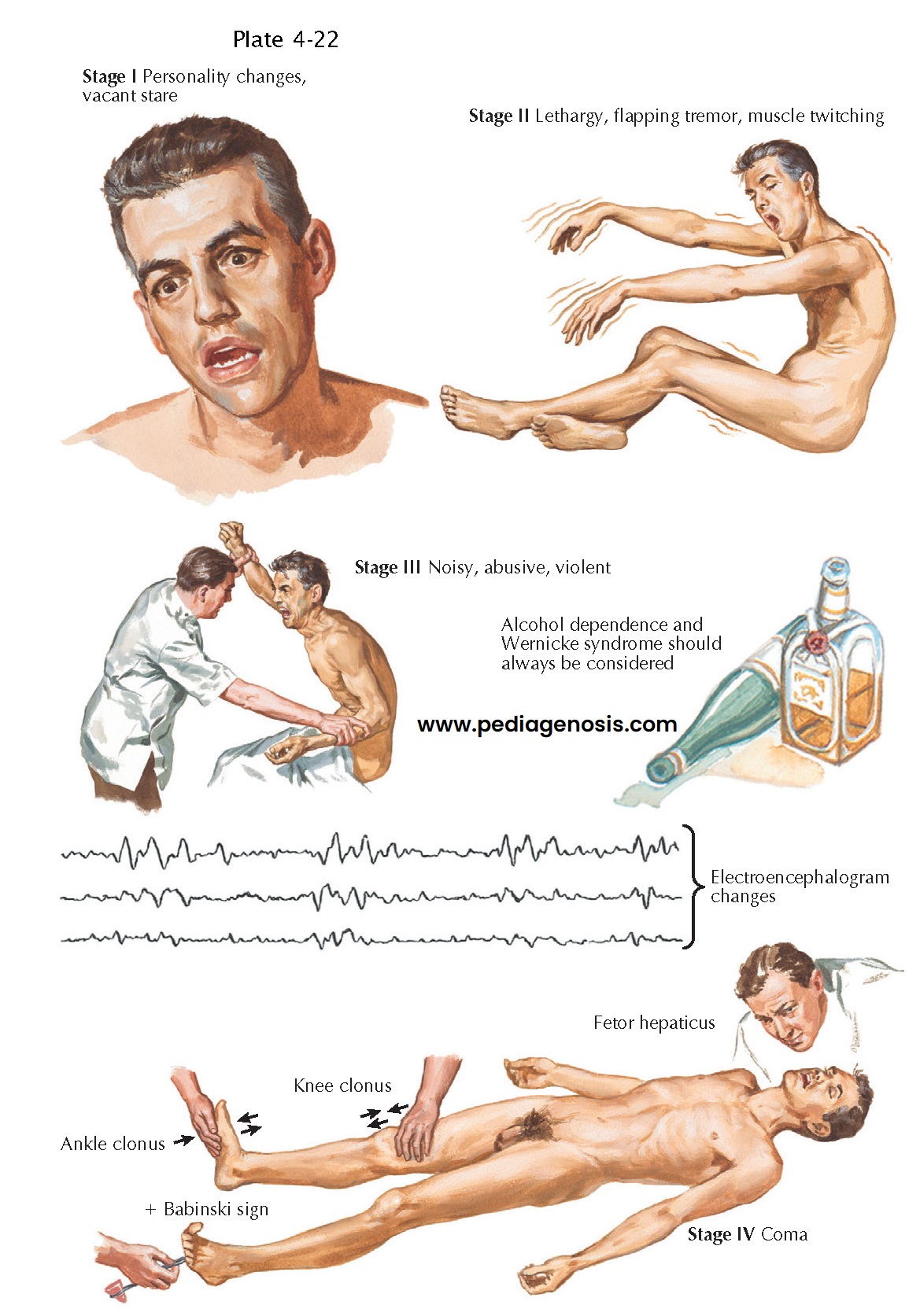
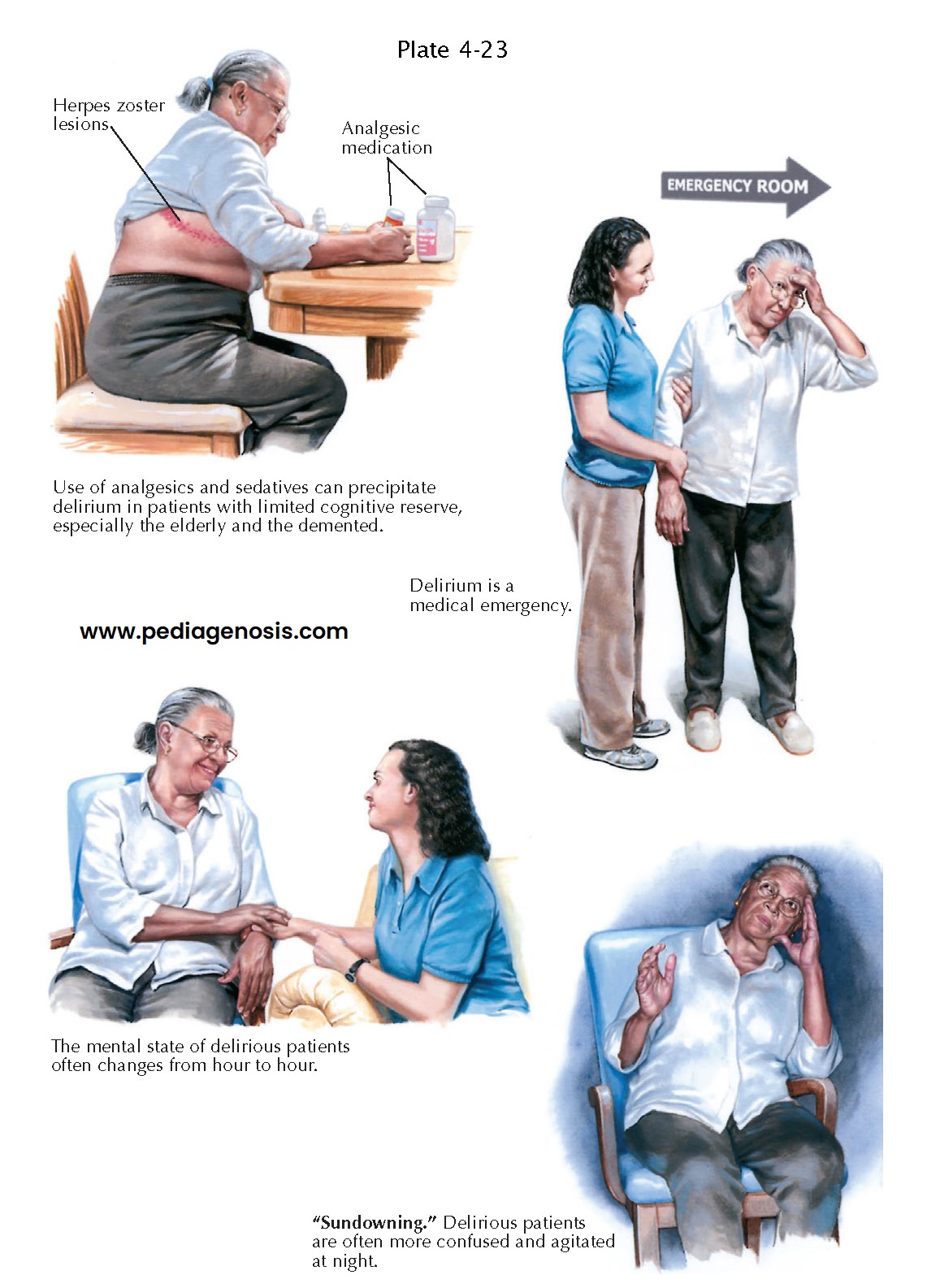
The presentation of
delirium is typically acute, over hours or days, and may persist for days to
months. There may be a prodromal phase, especially in elder patients,
including fatigue and lethargy, sleep disturbance, anxiety and/or depression,
or restlessness. The acuity of onset differentiates delirium from dementia in
most cases, although delirium in a demented patient may be difficult to detect,
especially early in the course. More-over, the severity of confusion may
fluctuate through-out the day, becoming particularly more prominent toward
night-time. Initially, there may be a subtle change in mental clarity,
inattention, and disorientation before more obvious behavior changes take
place. The patient is often very distractible, unable to maintain a cohesive train of thought or action. Patients are typically disoriented
to time. In more advanced cases, patients may become more obviously drowsy
and lethargic, even obtunded. However, the opposite may occur in some forms
of delirium, where the patient becomes hypervigilant, irritable, and
agitated, as seen in alcohol withdrawal. Hallucinations may occur. Cognitive
deficits, including amnesia, aphasia, agnosia, and apraxia may also appear.
Other clinical manifestations may include emotional lability, disturbance of
sleep cycle, motor restlessness, and sometimes motor signs, such as
asterixis, myoclonus, or action tremor. In the elder patient, the most
common presentation is of a withdrawn, quiet state that may be easily mistaken for depression.
Delirium is often
misattributed to psychiatric diagnoses— usually depression and catatonic schizophrenia
in hypoactive deliriums, and personality disorders and psychosis in hyperactive
deliriums. A patient with a first-episode psychosis or mania should be of
typical age, that is, a young adult, and should appear generally well, not diaphoretic,
flushed, befuddled, jaundiced, or clumsy. Psychiatric illness usually does NOT
account for disorientation, and does NOT cause motor symptoms or fevers.
Fluctuations in degree of alertness, variable motor signs, and uneven cognitive
performance are expected in delirium and do not signify a manipulative
personality. Use of antipsychotic medication may enable care, shorten duration
of delirium, and improve mortality,
even when the underlying cause is not psychiatric.
Psychiatric illness is a
diagnosis of exclusion for delirium and should be confirmed with a psychiatric
consultant when suspected. Similarly, if a delirious patient is under
psychiatric care, neurologic consultation should be obtained. Frontal brain
tumors, multiple sclerosis, epilepsy, encephalitis, and dementia can all have
delusions, hallucinations, mania, and aggression as manifesting signs.
Repeating sequences of odd behavior, indifferent attitude, amnesia, atypical
age, absence of prior or family history of mental illness, and presence of
primitive reflexes indicate more screening for neurologic disease.
Substance abuse very
frequently leads to various confusional presentations. The use of illicit
substances and overuse of alcohol are usually denied in medical settings;
however, ingestion of toxins and drug overdose, either recreational or
suicidal, should be considered in all cases of delirium. Alcohol,
barbiturates, and benzodiazepines all have life-threatening withdrawal
syndromes, as well as syndromes of intoxication. Antipsychotics are not a
treatment for withdrawal syndromes. Replacement therapy and controlled taper
for alcohol, benzodiazepine, and barbiturate-dependent patients are lifesaving.
Very rarely, anti–N-methyl-d-aspartate receptor (NMDAR) encephalitis, a
novel and significantly underdiagnosed diffuse encephalopathy, manifests
primarily (80%) in women with a combination of psycho- sis, including
catatonia, as well as dyskinesias, memory deficits, and convulsions. The
abnormal movements are varied, often including oral-lingual-facial akathisia
but also choreoathetosis, dystonia, oculogyric crisis, dystonia, rigidity, and
opisthotonos. Often, there is a less than 2-week history of a prodromal febrile
illness, including headache and respiratory or gastrointestinal symptoms. This
anti-NMDAR encephalitis is either a paraneoplastic disorder, secondary to an
underlying ovarian teratoma, or a primary autoimmune disorder occurring in
young adults or children. This is potentially reversible if recognized early
and treated with surgery and/or immunosuppression. Prognosis largely depends on
adequate immunotherapy and, in paraneoplastic cases, complete tumor removal.
Regardless of the
individual case, a comprehensive history, examination, and review of the
medical record must be completed to determine the underlying cause(s). Seizures
and focal signs on examination require brain imaging (magnetic resonance
imaging [MRI]/computed tomography [CT]) and/or electroencephalography (EEG) to
assess for acute structural lesions, infection, or inflammation. The nature of
the patient’s underlying medical condition requires standard laboratory tests,
including blood cultures as well as cerebrospinal fluid examination to
demonstrate evidence of possible systemic infections, electrolyte disturbance,
volume depletion, liver failure, uremia, thyrotoxicosis, and other systemic
disorders.
The examiner must
consider potential permanently damaging conditions, such as thiamine deficiency
(Wernicke encephalopathy), herpes encephalitis, or NMDAR encephalitis, all
requiring emergent therapy. A careful review of medications and toxicology
screens is essential. Drug toxicity accounts for 30% of delirium cases;
over-the-counter drugs, such as diphenhydramine, require attention, and other
specific drug syndromes exist
as well. When no mechanism is identified for the acute personality change,
particularly in young women, abdominal/pelvic imaging studies as well as
anti-NMDAR autoantibodies must be evaluated in serum or cerebrospinal fluid to
exclude anti-NMDAR encephalitis.
Antipsychotic medications
can precipitate the neuroleptic malignant syndrome, a triad of acute
confusion, rigidity, and hyperthermia. Antipsychotic medications, often
useful for behavioral control of an agitated patient, may also cause their own behavioral
syndrome of severe motor restlessness, or akathisia, which is usually
accompanied by markedly increased muscular tone and cramping. Combinations of
antidepressants, migraine medications, and some antibiotics can trigger the serotonin
syndrome, causing a triad of confusion, autonomic instability, and clonus. Lithium, along with other narrow-window
therapeutic drugs, such as digitalis, can cause delirium even with levels in
the recommended therapeutic range. Lithium toxicity usually manifests with vomiting
or diarrhea, severe tremors, and ataxia, whereas digitalis toxicity often
causes paranoia and hallucinations. Serum levels of any drug the patient is
taking should be checked when available, and all nonessential medications
should be held.
Treatment of delirium requires identification of the underlying medical problem, judicious use of psychoactive medication to keep the patient and others safe from aberrant behavior, and maintaining a peaceful environment. The presence of delirium is a well-established source of increased morbidity and mortality—and a syndrome in urgent need of a diagnosis.