OBSTETRIC
LACERATIONS I—VAGINA, PERINEUM, VULVA
Nearly every primiparous birth results in at
least a minor injury to the soft parts of the vagina, perineum, and vulva.
Traditionally a timely median or mediolateral episiotomy was believed to reduce
the likelihood that such tears will be extensive, but the role of routine
episiotomy has come under question. In spite of prophylactic incisions, bad
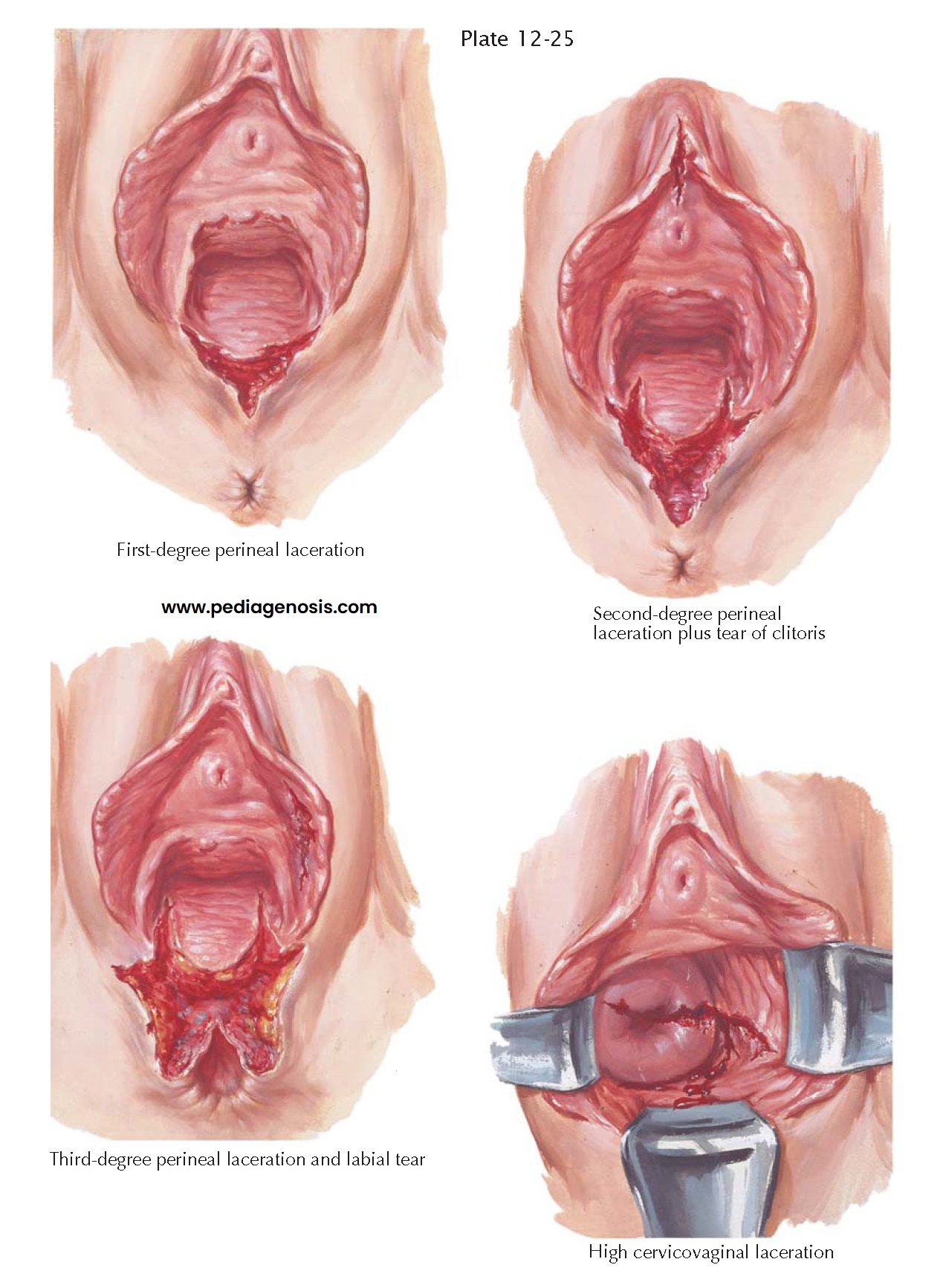
lacerations occur, which vary greatly in degree and direction. The simplest
type is a first-degree perineal laceration that extends posteriorly toward the
anus through the vaginal epithelium and perineal skin. Occasionally, the
inferior borders of the labia are also torn, and lateral retraction from the
cut surface causes gaping of the wound. Bleeding may be brisk, but
self-limited, although no vital structures have been damaged. It is important
to make a thorough examination of the adjacent tissues to rule out the presence
of occult damage elsewhere.
Second-degree lacerations involve the skin, vaginal epithelium, and the superficial muscles of the perineum but not the fibers of the external anal sphincter. They often extend upward along the sides of the vagina, producing a triangular defect because of retraction of the superficial perineal muscles. At the lower margin of a second-degree tear, the capsule of the external anal sphincter bulges upward into the wound. Concomitant lacerations of the anterior vagina, clitoris, prepuce, urethra, and labia are frequently present.
A third-degree perineal
laceration is a far more serious injury because of the threat of future
interference with normal bowel function. In this instance, the skin, vaginal
epithelium, and perineal body are torn, and the external anal sphincter is
ruptured anteriorly with retraction of its severed ends. Although the perineum
receives the main expulsive force and is there- fore more often lacerated, the
incidence of damage to the anterior wall increases proportionately. Superficial
epithelial wounds, perforation of the bladder, or even avulsion of the urethra
may result.
A tear that includes the
rectal mucosa or extends up the anterior rectal wall to compromise the internal
sphincter is referred to as a fourth-degree laceration. Third- and
fourth-degree lacerations commonly produce fecal incontinence if untreated and
are slow to heal. The puckered scar tissue, which forms in wounds that heal by
second intention in this area, is often painful.
Inspection of the cervix
and upper vagina after delivery, regardless of the presence or absence of
external wounds, should always be considered. Cervical lacerations originating
at this time may be the source of problems, including postpartum bleeding and
cervical insufficiency. If the tear extends to the vaginal fornices, as it often
may, the end result may be dyspareunia or urinary incontinence due to downward
pull on the internal vesical sphincter. More acute symptoms are hemorrhage,
hematoma, or infection followed by purulent leukorrhea.
The early and late clinical manifestations of all these injuries serve to emphasize the necessity of instituting prompt surgical treatment. Transfusions may be necessary to combat hemorrhage and shock if bleeding is significant. Sutures should be carefully and economically placed, which, in the difficult cases, usually requires the services of an assistant for adequate exposure. Upon completion of the third stage of labor, all lacerations should be repaired. In the case of third-and fourth-degree lacerations, this means that the severed fibers of the rectal sphincters are reunited and further strengthened by reapproximation with either an end-to-end or overlapping technique. To provide additional support, plication of the levator muscles in the rectovaginal space has been advocated in the past. Such repair may be done safely immediately following delivery, though data on the advisability or success of such an approach is lacking. Primary repair is always preferable because, in the event of failure, subsequent corrective procedures offer a much more limited prognosis.