Pediatrics:
Eating Disorders
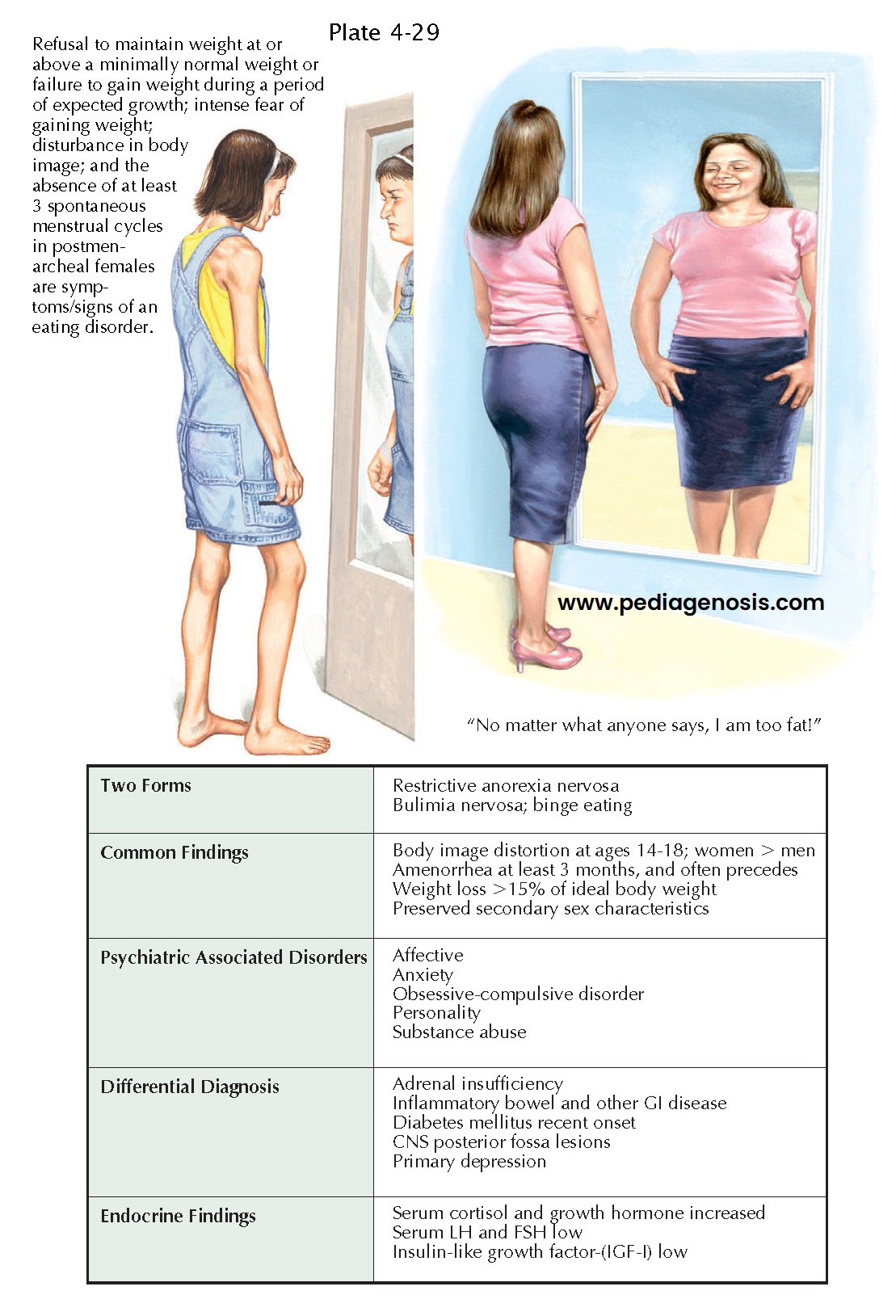
Eating disorders occur in adolescents who have intense preoccupation with body weight and shape and impaired eating habits. Patients have distorted thoughts and emotions concerning their appearance as well as abnormal eating behaviors; these lead to alterations in body composition and functioning occur. The etiology of eating disorders is multifactorial and includes a genetic component, sociocultural pressures to be thin, and the promotion of dieting. Performers and athletes, particularly those participating in activities that reward a lean body (e.g., gymnastics, running, wrestling, dance, or modeling) are at particular risk. Girls who feel most negatively about their bodies at puberty are at highest risk for the development of eating difficulties. The prevalence of eating disorders is variably reported, 0.8% to 14%. Their epidemiology has gradually changed concomitantly in the United States and world-wide, with an increasing prevalence in males, younger age groups, minority populations in the United States, and now countries where eating disorders uncommonly occurred. Acculturation to Western values is a risk factor for eating disorders in U.S. immigrants.
Clinical
Presentation. There
are two primary eating disorders: anorexia nervosa (AN) and bulimia
nervosa (BN). A third category, eating disorder not otherwise specified (ED
NOS), represents those disorders not meeting criteria for AN or BN. ED NOS
includes more patients than the other two primary diagnoses.
Anorexia nervosa is
characterized by fear of gaining weight, low body mass index, denial of current
low weight and its impact on health, and amenorrhea. Prevalence is highest in
teenage girls; up to 0.7% may be affected. Behaviors used to reduce weight
include restricting meals and calories, hyperexercising, self-induced vomiting
(purging), and use of diet pills or laxatives. Psychiatric and personality
disorders, such as depression, anxiety disorders, obsessive-compulsive dis-
order, and perfectionism, are common.
Bulimia nervosa patients
have regular episodes of uncontrolled overeating (binge eating) associated with
extreme measures to counteract the feared effects of the overeating, such as
occur with AN. Approximately 90% of BN patients are women who become
symptomatic in late adolescence; their binge eating typically begins in the
context of dieting. As BN patients may have normal weight or be overweight,
this diagnosis is more difficult to entertain. Although BN patients experience
weight variations, they rarely approach the low AN weights. Higher obesity
rates, mood disorder, sexual and physical abuse, parental obesity, and
substance misuse exist in BN patients.
Short-term medical
complications include electrolyte disturbances, esophageal tears, gastric
disturbances, dehydration, orthostatic blood hypotension, and cardiac
dysfunction and sometimes require hospitalization. Long-term medical
complications typically resulting from chronic malnutrition include growth
hormone changes, hypothalamic hypogonadism, bone marrow hypoplasia, and brain
structural abnormalities.
Diagnosis. Pediatricians, child and adolescent
psychiatrists, child psychologists, child-trained social workers, counselors,
and clinical nurse specialists are best trained to accurately diagnose eating
disorders. Because these can affect every organ system, and the medical
complications can be serious to life-threatening, a comprehensive history and
physical examination is required.
Treatment. This requires that individual,
family, medical, and nutritional aspects be addressed. The initial therapeutic goal for AN
patients is the restoration of physical health. Family therapy provides the
most promising results in adolescent AN and BN. Cognitive-behavioral
therapeutic strategies are helpful in BN for behavioral changes, for example,
for bingepurge reduction. No medications are approved by the FDA for AN
treatment. Although pharmacotherapy is sometimes prescribed, it is typically
targeted at comorbid depression and anxiety. Selective serotonin reuptake
inhibitor antidepressants may reduce binge eating episodes and purging.
Course. Although most eating disorder individuals recover completely or partially, about 5% die and 20% develop a chronic eating disorder. Even after recovery, there are high rates of residual psychiatric illness, pre-dominantly depression and anxiety. The potential for significant growth retardation, pubertal delay or interruption, and peak bone mass reduction are significant medical problems for adolescents in contrast to adults. Young anorectic women have an increased risk of fractures later in life. Eating disorders in adolescents are identified as the psychiatric condition with the highest mortality rate; however, these are lower than those historically reported. In a recent meta-analysis, the mortality rate among AN adolescents was 1.8% compared with 5.9% when adults and adolescents were considered together. Mortality is most often attributable to the complications of starvation or to suicide.