Pediatrics:
Attention-Deficit/Hyperactivity Disorders
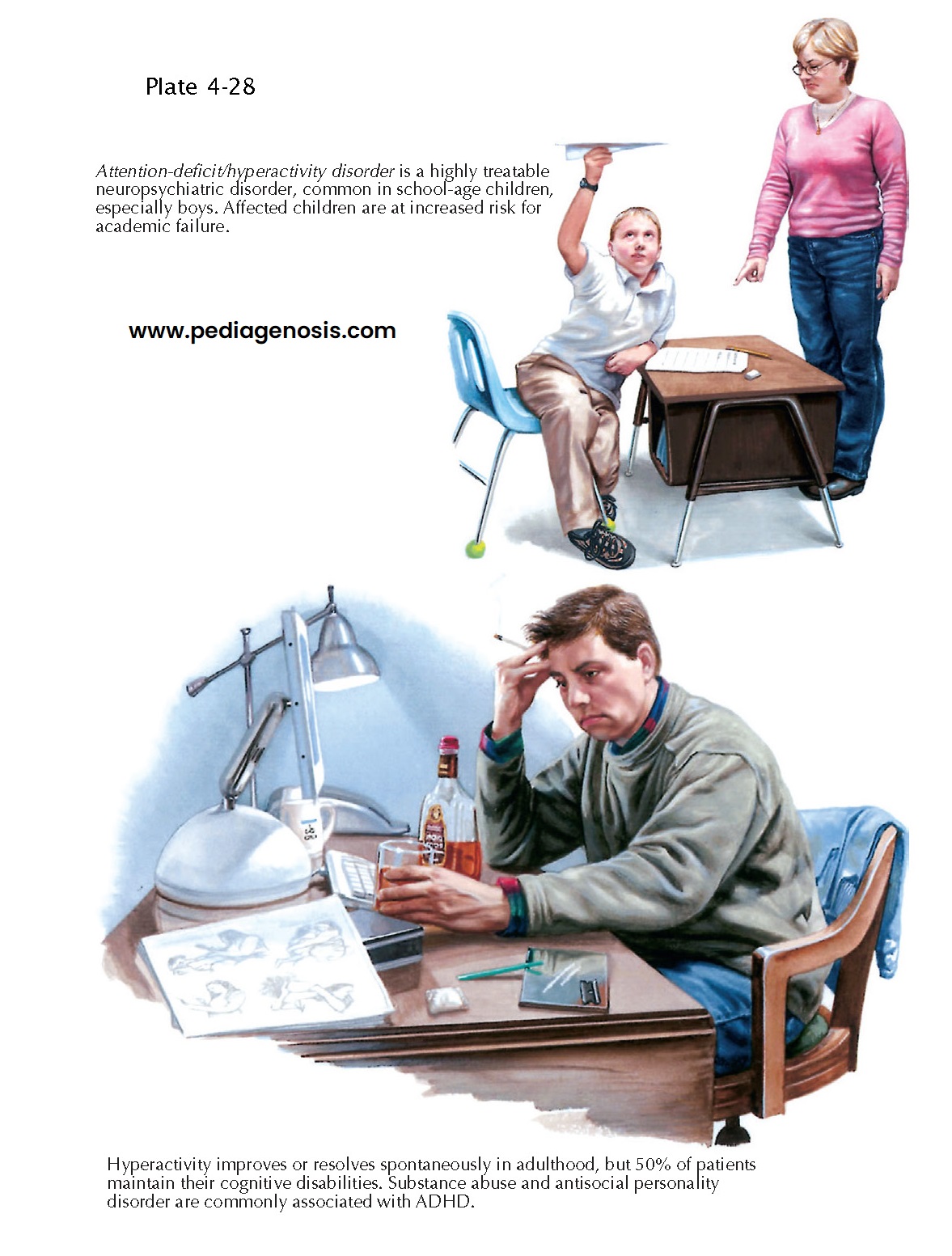
The attention-deficit hyperactivity disorders (ADHD) are a group of childhood, adolescent mental health problems characterized by difficulty controlling attention, motivation, and behavioral impulses. These are common childhood psychiatric conditions, affecting 5% to 12% of children worldwide. More common in boys, there is increasing evidence that the principal cause of ADHD is genetically based. A greater American prevalence may result from varied diagnostic practices and cultural expectations. ADHD is related to differences in prefrontal cerebral cortex structure and function. These are important for controlling organization, planning, attention, and impulses. Maternal drinking or smoking during pregnancy, low birth weight, chemical injuries to the brain (e.g., lead poisoning), and severe child neglect are associated with ADHD.
Clinical
Presentation. Four
types of ADHD are recognized. ADHD, as the predominantly inattentive
type, is characterized by a persistent pattern of poor attention and lack of
motivation, particularly when sustained mental effort is required (such as for
schoolwork or homework). These children are often described as “daydreamers” or
“spacey.” ADHD, as the predominantly hyperactive/impulsive type, is
characterized by a persistent pattern of overactive behavior (such as being
fidgety, restless, walking around without permission in class, or talking
excessively when it is important to behave quietly), as well as impulsive
behavior (such as difficulty waiting, not stopping to think before acting or
blurting out answers). ADHD, as the combined type is characterized by
both inattention and hyperactivity/impulsivity. To meet such diagnoses, these
problems must be more frequent and severe than children normally exhibit, start
before age 7 years, be present for at least 6 months, be noted in two or more
settings, and impair the youth’s function at home, at school, or with peers. A
child with ADHD observed in a highly structured environment or engaged in a
stimulating activity (i.e., playing video games), may not exhibit any symptoms.
Unstructured, boring, and minimally supervised environments tend to enhance
typical ADHD symptoms.
If some of the above
problems are present, but not enough to meet the diagnoses, the disorder is
called attention-deficit/hyperactivity disorder, not otherwise specified.
Diagnosis. Child and adolescent psychiatrists,
pediatricians, child psychologists, child-trained social workers, counselors,
and clinical nurse specialists are best trained to accurately diagnose ADHD.
The evaluation typically takes several hours, requiring input in the form of
interviews and/or questionnaires from parents/caregivers and teachers as well
as a careful mental status examination of the child. There are no specific
blood tests, imaging studies, or other medical tests to diagnose these
disorders.
Treatment. The cornerstones of treatment are
education about the disorder, appropriate school class placement, and
medication. Medications are the most effective treatment for ADHD, with
stimulant medications the first line of treatment. Stimulant medication is
effective because it works by “stimulating” the brain, presumably the prefrontal
cortex that controls attention, motivation, and behavioral impulses.
Tutoring the child in
effective study skills (such as setting goals, planning ahead, self-rewarding)
is helpful.
At school, accommodations
for inattention can be requested. These include frequent reminders to stay on
task, reducing distractions, rewarding persistence, providing reminders to
complete assignments (e.g., turning in homework), and giving extra time to
complete work. Other school accommodations can be requested, such as providing
opportunities for physical activity or “boredom breaks” during the day,
providing a variety of interesting approaches to learning, giving rewards for
control of behavioral impulses, and giving consequences for failing to control
behavioral impulses.
Other useful strategies
include providing a predictable, structured environment at home and a
supportive environment for homework, such as a quiet place to work, breaking
tasks into small portions, while offering small rewards for completing each
item. About one third
of ADHD youths demonstrate learning and/or language disabilities. These are
identified through psycho-educational testing, and remediated with tutoring
and/or speech therapy. Testing (and remediation if needed) should be requested
from the school.
Course. ADHD responds well to the above treatments. About one third of children grow out of ADHD in the teen or early adult years. The remaining two thirds of children may continue to need support as they grow into adulthood, including ongoing use of medication as well as accommodations and supports at school, at work, and at home. If untreated, ADHD can go on to cause significant problems, including failure at school, injuries and accidents, substance abuse, other risky behaviors, difficult relationships with parents and peers, and poor self-esteem.