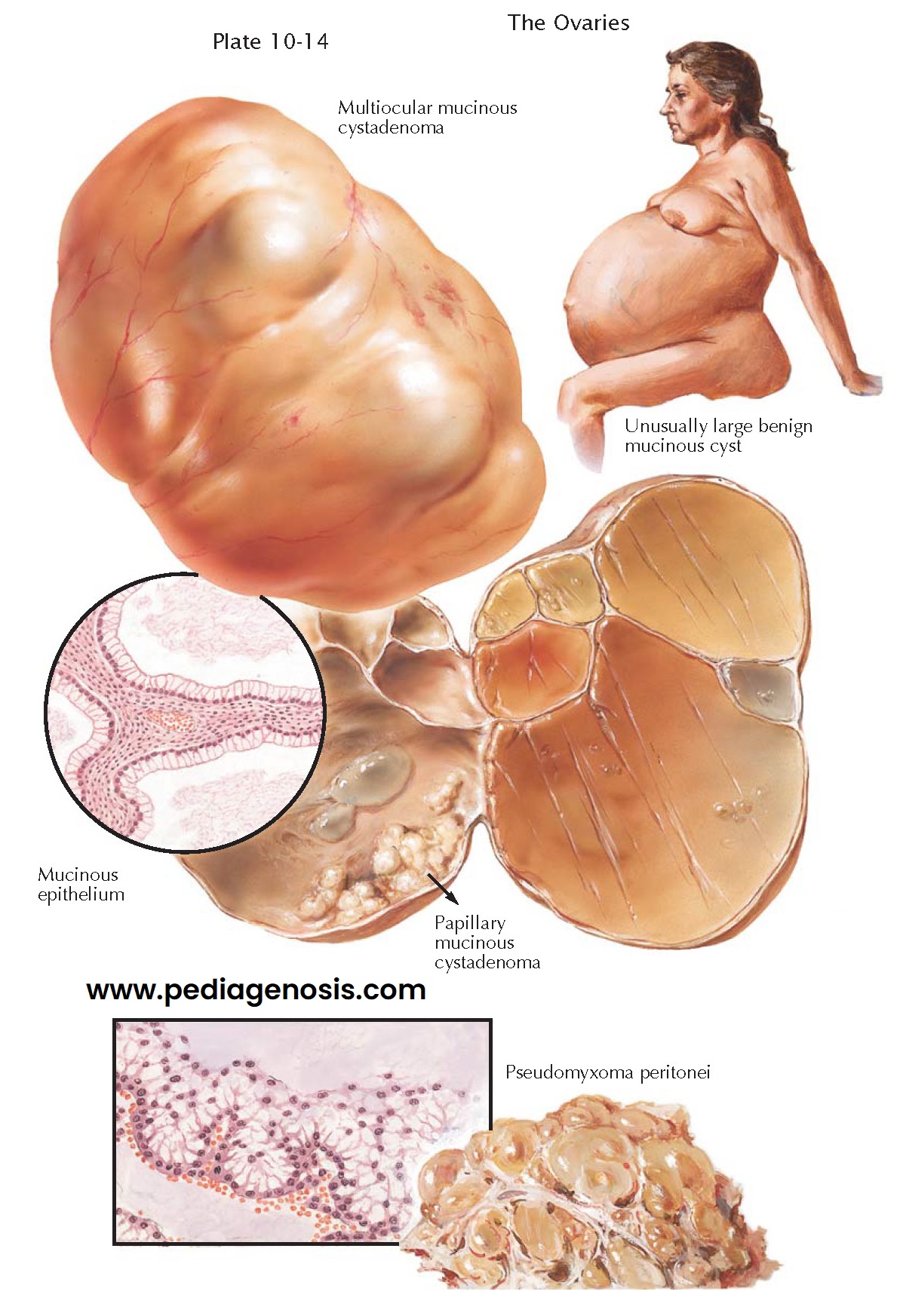
MUCINOUS CYSTADENOMA
Mucinous (pseudomucinous) cystadenomas are cystic neoplasms of the ovary in which the lining epithelium is mucus-producing. They are usually unilateral, multilocular, lobulated, smooth-surfaced, tensely cystic, pedunculated, and benign. They represent the most common type of ovarian cyst, occurring with slightly greater frequency than the serous cystadenomas. Usually, they are encountered during the reproductive years (20 to 50 years), rarely before puberty or after the menopause. In contrast to serous epithelial growths, they are less likely to be bilateral (10%) or papillary (10%) and are rarely malignant (5% to 15%). Mucinous cystadenomas may be minute in size or may fill the abdomen: mammoth ovarian cysts are apt to be of the mucinous type. Generally, they are recognized and are removed before reaching a diameter of 15 to 30 cm. Torsion of the pedicle is common (20%). Ascites is rare but may occur. Hydrothorax and hydroperitoneum, as encountered in Meigs syndrome, have been described. Intracystic hemorrhage, secondary suppuration, and spontaneous rupture are rare. Penetration of the capsule, with implantation and growth of mucinous epithelium in the peritoneal cavity, may cause pseudomyxoma peritonei. The rate of growth is generally slow. Rupture of a cyst by trocar, aspiration, or handling should be avoided. Unilateral removal of ovary and tube is the therapy of choice, at which time the specimen must be carefully examined for evidences of localized, firm infiltrations in the cyst wall.
Grossly, the outer surface of mucinous cysts appears smooth, lobulated,
glistening, and grayish white or whitish blue in color. The cut surface may
present a variety of architectural patterns, including a unilocular cyst with
internal, sickle-shaped ridges representing the remnants of previous
interlocular septa; a multilocular, semisolid neoplasm, with chambers of
varying size and honeycombed cystic aggregates projecting into the lumen; or a
more solid tumor composed of numer- ous minute compartments that present a
spongelike appearance. Internal papillary excrescences are uncommon (10%). The
cyst wall is fibrous and of varying thickness. Septa are firm, fibrous or
adenomatous, complete or incomplete. The characteristic fluid is mucoid, viscid,
and transparent or cloudy. As a result of bleeding, the fluid contents may
assume a red, tan, brown, or black color.
Microscopically, the connective tissue capsule is composed of an outer
layer of dense, fibrous tissue and an inner zone, which is looser and more
cellular. Evidences of localized degeneration may be noted, including edema,
inflammation, necrosis, fatty acid deposits, and calcification. The dividing
septa are extensions from the inner zone of connective tissue. A
well-differentiated, single-layered epithelium lines the cyst walls and
trabeculae. It invaginates into the connective tissue stroma to give an
adenomatous appearance. The epithelial lining is composed of tall columnar
cells, with deeply staining basal nuclei and abundant acidophilic, finely
granular cytoplasms. Actively secreting goblet cells are scattered irregularly
between the columnar cells.
Pseudomyxoma peritonei refers to the secondary implantation on the
peritoneum of mucinous tissue, with subsequent local invasion, proliferation,
and overproduction of thick, gelatinous, mucinous material, which may fill the
pelvis, abdomen, and subphrenic spaces. Pseudomyxoma peritonei may follow
rupture of a mucinous cystadenoma of the ovary or a mucocele of the appendix.
Recent histologic studies suggest that in the majority of patients the appendix
is the primary tumor source. In rare cases, metaplasia by the cells of the
peritoneal surface may account for this tumor.
Clinically, pseudomyxoma peritonei may give rise to a progressive enlargement of the abdomen, evidences of increased abdominal pressure, interference with bladder and bowel function, and cachexia. The condition is progressive and, though histologically benign, may cause a fatal outcome owing to mechanical interference. The rate of growth may be rap d, or the progress may be drawn out over many years.