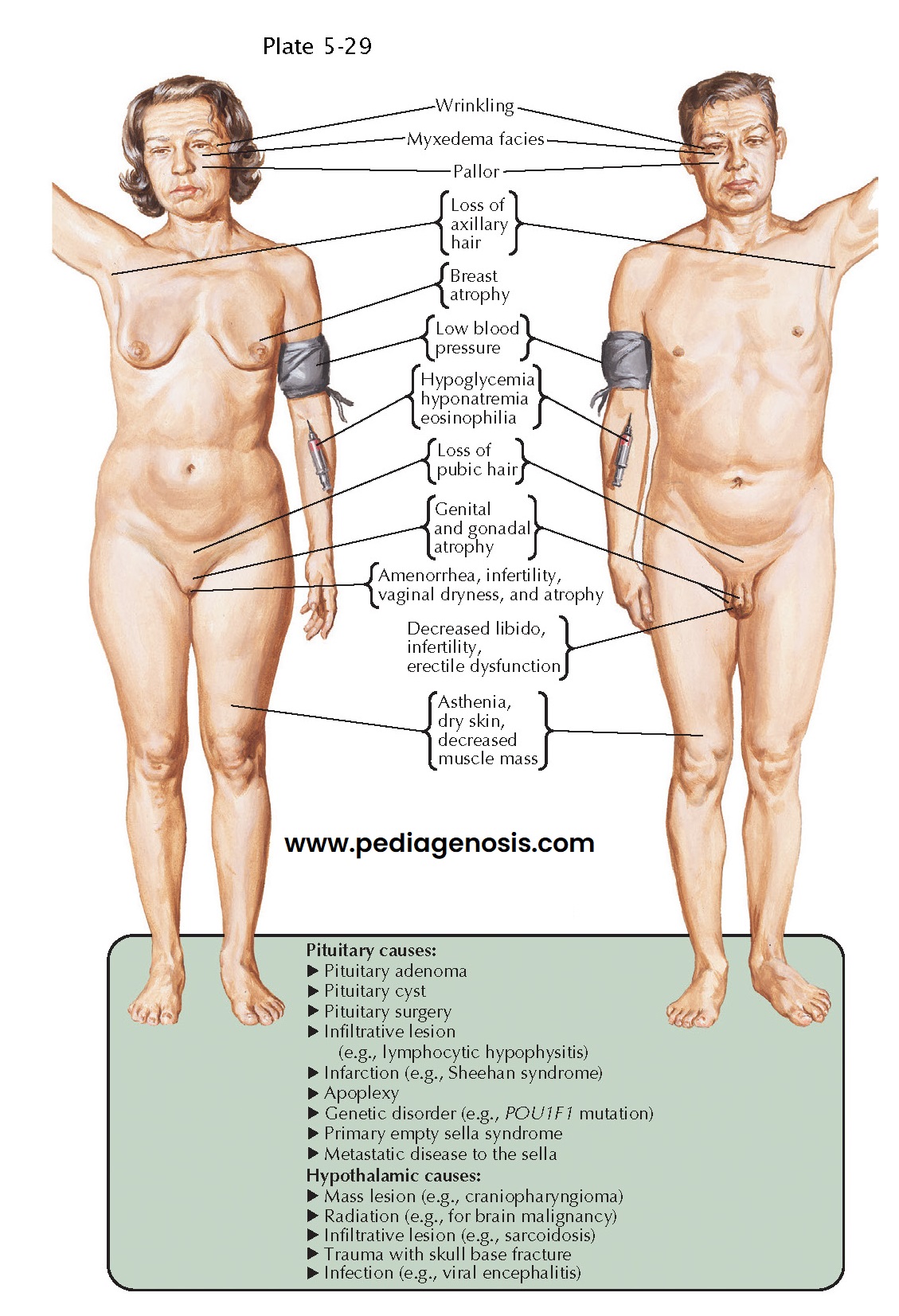
Anterior Pituitary Hormone Deficiencies
There are six types of secretory cells present in the adenohypophysis, including somatotrophs (synthesizing growth hormone), lactotrophs (producing prolactin), mammosomatotrophs (synthesizing both growth hormone and prolactin), thyrotrophs (producing thyrotropin), corticotrophs (synthesizing corticotropin), and gonadotrophs (synthesizing both follicle-stimulating hormone and luteinizing hormone). The synthesis and release of these hormones is well orchestrated under the influence of hypothalamic hormones (most of which are stimulatory and some of which are inhibitory) as well as systemic (endocrine) negative feedback mechanisms, aimed at maintaining homeostatic control.
A wide variety
of conditions may cause dysfunction of the hypothalamus or pituitary, leading
to selective or universal, partial or complete, acute or chronic loss of
adenohypophyseal hormone secretion (anterior hypopituitarism). Any
space-occupying lesion impinging on the anterior pituitary, stalk, or
hypothalamus may lead to hypopituitarism. In adults, the most common mass
lesion in the area of the sella is a benign pituitary adenoma. However, many
other neoplasms (including craniopharyngioma, meningioma, chordoma, metastases,
or lymphoma), cystic lesions (including Rathke’s cleft cyst or arachnoid cyst),
infiltrative (hemochromatosis), inflammatory (hypophysitis, sarcoidosis) or
infectious disorders, aneurysm, infarction, primary empty sella, radiation
therapy, trauma, surgery, or genetic conditions may all cause hypopituitarism. The
underlying cause of hypopituitarism may influence the pattern of hormone loss. Gonadotropin
deficiency and growth hormone deficiency tend to occur first in patients with
pituitary adenomas or those who have received
radiation therapy to
the hypothalamus and sella, while thyrotropin and
corticotropin function tend to be spared until later in the course of these
conditions. In contrast, corticotropin and thyrotropin deficiency frequently
occur first in patients with lymphocytic hypophysitis.
Gonadotropin
deficiency presents as lack of pubertal development in adolescents, who generally
develop a eunuchoid habitus. If the onset of gonadotropin deficiency occurs in
adulthood, patients present with loss of gonadal function, including
oligomenorrhea or amenorrhea in women, and erectile dysfunction in men. In
addition, low libido and infertility may occur in patients of both genders.
Patients may also experience loss of body hair (particularly in the presence of
concurrent corticotropin deficiency), fine facial wrinkling, loss of bone
calcium leading to increased fracture risk, and hot flashes. Women may also
experience breast atrophy, vaginal dryness, and dyspareunia. Men may note loss
of stamina, increased body fat, decreased lean body mass, and decreased
testicular size. Prolactin deficiency may result in failure of lactation
postpartum.
Growth
hormone deficiency leads to decreased linear growth if it occurs in childhood or adolescence.
In adulthood, loss of growth hormone secretion is more subtle, but may be
associated with fatigue, decreased exercise capacity and muscle strength,
abnormal body composition (decreased lean body mass, loss of bone calcium, and
gain in body fat), dyslipidemia, insulin resistance, increased cardiovascular
risk, and poor quality of life.
Thyrotropin
deficiency leads to central hypothyroidism, including fatigue, lethargy, weight gain,
bradycardia, dry skin, myxedema, anemia, constipation, muscle aches, decreased
relaxation phase of Achilles reflexes, and cold intolerance.
Corticotropin
deficiency leads to central hypoadrenalism, which is potentially the most life
threatening of all pituitary hormone deficiencies. These patients often
exhibit fatigue, weight loss, nausea and vomiting, orthostatic hypotension and
dizziness, and diffuse arthralgias. Notable is the lack of cutaneous and
mucosal hyperpigmentation, in contrast to patients with primary adrenal
insufficiency (Addison disease). These patients may also present acutely with
shock unresponsive to volume expansion and pressors. Eosinophilia and
hyponatremia may be present. However, hyperkalemia is absent, because
aldosterone deficiency does not occur.
Once diagnosed, target organ hormone replacement therapies are instituted. In particular, glucocorticoid replacement may prove lifesaving in patients presenting in adrenal crisis. Levothyroxine is used to replace central hypothyroidism, and sex steroid replacement is used to replace patients with central hypogonadism. However, if fertility is of interest, gonadotropin therapy is used, including human chorionic gonadotropin and follicle-stimulating hormone. Growth hormone replacement may also be considered. Despite seemingly adequate replacement therapies, patients with hypopituitarism are at increased risk of cardiovascular mortality, the underlyi g reasons still being a matter of considerable debate.