INNERVATION OF
STOMACH AND DUODENUM
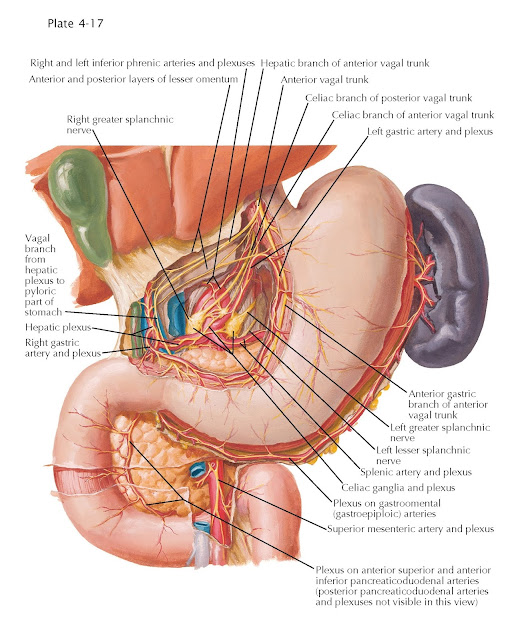
The stomach and duodenum are innervated by the visceral efferent sympathetic and parasympathetic nerves, along which run visceral afferent fibers.
The sympathetic supply to the
stomach emerges in the anterior spinal nerve roots as presynaptic axons
projecting from cells within the intermediolateral cell column of the
spinal cord, particularly from the 5th to the 9th or 10th thoracic segments.
They are carried from the spinal nerves in white rami communicans that
pass to the adjacent sympathetic ganglia located along the length of the
sympathetic trunk. The sympathetic axons that will supply the stomach
pass through the ganglia without synapsing and travel along the thoracic
vertebrae as the thoracic splanchnic nerves, which pass through the
diaphragm posteriorly to reach celiac ganglia. Generally, these axons
will form synapses with postsynaptic nerve cells in the celiac and superior
mesenteric ganglia. The postsynaptic axons of these cells are conveyed to
the stomach and duodenum in the celiac plexus and the superior
mesenteric plexus. We will concentrate on the former, as it is the primary
nerve supply to the stomach and proximal duodenum. The axons of the celiac
plexus adhere to the walls of the arteries that arise from the celiac arterial
trunk; they may be referred to as the hepatic plexus, splenic plexus, or
left gastric plexus, depending upon which artery they follow. The
sympathetic axons of each plexus run alongside presynaptic parasympathetic
axons and visceral afferent axons.
 |
| AUTONOMIC INNERVATION OF STOMACH AND DUODENUM |
Subsidiary plexuses from the
hepatic arterial plexus are continued along the right gastric and gastroduodenal arteries and from the latter along the right gastroomental and anterior
and posterior superior pancreaticoduodenal arteries. The splenic
arterial plexus sends offshoots along the short gastric and left gastroomental
arteries.
The left gastric plexus consists
of one to four branches that accompany the artery and supply twigs to the
cardiac region of the stomach and communicate with offshoots from the left
phrenic plexus. Other filaments follow the artery along the lesser curvature of
the stomach between the layers of the lesser omentum to supply adjacent parts
of the stomach. They communicate profusely with the right gastric plexus and
with gastric branches of the vagus. The nearby phrenic plexuses assist
in supplying the cardiac end of the stomach. A filament from the right
plexus sometimes turns to the left and passes to the region of the cardiac
orifice, whereas the left phrenic plexus supplies a constant twig to the
cardiac orifice. A delicate branch from the left phrenic nerve (not
illustrated) supplies the cardia.
The splenic plexus gives off
subsidiary nerve plexuses around its pancreatic, short gastric, and left
gastroomental branches, and these supply the structures indicated
by their names. A filament may curve upward to supply the fundus of the
stomach.
The hepatic plexus gives off
subsidiary plexuses along all its branches. These, following the right gastric
artery, supply the pyloric region, and the gastroduodenal plexus accompanies
the artery between the first part of the duodenum and the head of the pancreas,
supplying fibers to both structures and to the adjacent parts of the common
bile duct. When the artery divides into its anterior superior
pancreaticoduodenal and right gastroomental branches, the nerves also
subdivide and are distributed to the second part of the duodenum, the
terminations of the common bile and pancreatic ducts, the head of the pancreas,
and the parts of the stomach. The part of the hepatic plexus lying in the free
margin of the lesser omentum gives off one or more (hepatogastric) branches
that pass to the left between the layers of the lesser omentum to the cardiac
end and lesser curvature of the stoma h; they unite with and reinforce the
left gastric plexus.
The superior mesenteric ganglion
is primarily involved in supplying postsynaptic axons to the midgut organs.
It does supply the distal duodenum by means of axons that follow the anterior
and posterior inferior pancreaticoduodenal arteries to reach the duodenum and
pancreatic head.
The parasympathetic supply of the
stomach and duodenum arises in the dorsal vagal motor nucleus in the floor of
the fourth ventricle. The dorsal vagal motor nuclei contribute presynaptic
parasympathetic axons to the left and right vagus nerves, which leave
the jugular foramen to innervate thoracic and abdominopelvic organs. We will
ignore the activity of the vagus nerves in the thorax other than to mention
that the left and right vagus nerves closely associate with the esophagus and
interweave to produce the anterior and posterior vagal trunks, which
pierce the diaphragm alongside the esophagus to enter the abdominal cavity. The
anterior vagal trunk travels on the anterior aspect of the stomach and across
the hepatogastric ligament to innervate some of the liver and
gallbladder. Frequently, one branch, the greater anterior gastric nerve, is
larger than the others. The various gastric branches can be traced for some
distance beneath the serous coat before they sink into the
muscle coats, and although they communicate with neighboring gastric nerves, a
true anterior gastric plexus in the accepted sense of the term does not usually
exist. The pyloric branches (not illustrated) arise from the anterior vagal
trunk or from the greater anterior gastric nerve and run to the right between
the layers of the lesser omentum before turning inferiorly through or close to
the hepatic plexus to reach the pyloric antrum, pylorus, and proximal part of
the duodenum.
Small celiac branches run alongside
the left gastric artery to the celiac plexus, often uniting with corresponding
branches of the posterior vagal trunk. The posterior vagal trunk moves further
posteriorly from the esophagus to run into the nearby celiac ganglion. In
contrast to the presynaptic sympathetic axons entering the celiac ganglion, the
presynaptic parasympathetic axons do not synapse there but instead pass through
the ganglion to enter the celiac plexus. From there
these axons, alongside the postsynaptic sympathetic axons from the celiac
ganglion and viscerosensory axons, travel along branches of the celiac trunk,
the hepatic, splenic, and left gastric plexuses, to reach the foregut organs.
When these presynaptic parasympathetic axons reach the target organs, they
synapse with postsynaptic parasympathetic nerve cell bodies located within the
organs’ walls.
 |
| AUTONOMIC INNERVATION OF STOMACH AND DUODENUM: SCHEMA |
Viscerosensory activity related to
the stomach and duodenum is divided into two categories, visceral pain and
normal visceral reflexive stimuli. The stomach is insensitive to ordinary
tactile, painful, and thermal stimuli, although it responds strongly to
tension, ischemia, and chemical irritations as visceral pain. Visceral pain
fibers travel in a retrograde fashion along the sympathetic innervation of the
stomach; therefore, visceral pain axons traveling along the left gastric, right
gastric, left gastroomental, or right gastroomental plexuses would eventually
reach the celiac ganglion. Without synapsing, such an axon would continue along
the greater thoracic splanchnic nerves, through the sympathetic chain ganglia,
and then through the white rami communicans, anterior ramus, and spinal nerve.
At this time, being afferent, the axon would travel along the posterior root to
reach the spinal cord. Prior to reaching the spinal cord, the axon encounters
(but does not synapse within) its nerve cell body. The nerve cell bodies of
these viscerosensory axons are located in the posterior (dorsal) root ganglia.
Because these nerve cells are pseudounipolar, their axon extends from the
target tissue to reach the cell body but also proximally to reach the posterior
gray horn of the spinal cord.
Nonpainful, reflexive stimuli from
the stomach travel in a retrograde manner along its parasympathetic
innervation. Because all foregut organs receive their presynaptic
parasympathetic innervation via the vagus nerves, reflexive visceral afferents
from the stomach ascend along the vagus nerve to reach the brainstem and then
project to the inferior aspect of the solitary nucleus. The cell bodies for
these axons are located in the inferior vagal ganglion, which is located
near the point at which the vagus nerves exit from the right and left jugular foramina.





