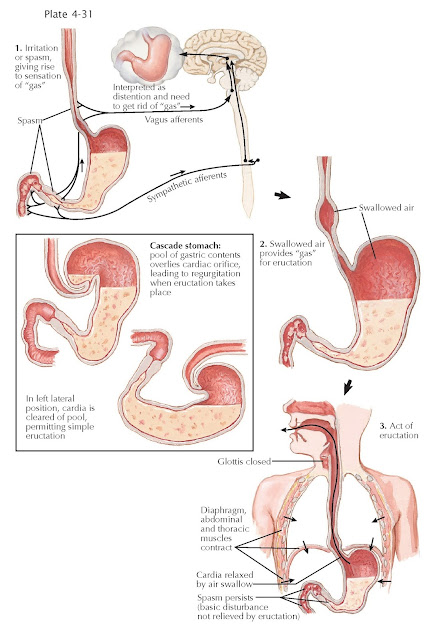
AEROPHAGIA AND BELCHING
Aerophagia is described as objectively observed or measured air swallowing. Aerophagia usually leads to troublesome repetitive belching. These symptoms must occur at least 3 times a week for over 6 months to be considered a functional gastrointestinal disorder by the ROME criteria, a consensus gastrointestinal guideline. Aerophagia with belching is seen more commonly in developmentally disabled or anxious persons but can be seen in any population.
There
are various pathophysiologic mechanisms by which aerophagia occurs. For one, a
person can swallow air and retain it in the esophagus. This can occur voluntarily
or in conditions in which the lower esophageal sphincter remains tight, such as
achalasia. Aerophagia occurs during normal daily activities such as swallowing
saliva; however, it can be exacerbated by certain lifestyle factors such as
rapid ingestion of food, smoking, chewing gum, or drinking carbonated
beverages. Physical activity with deep breathing, mouth breathing, and the use
of a continuous positive airway pressure device can also lead to increased
aerophagia. Hyperventilation when nervous or mouth breathing due to nasal or
sinus disorders also is a common cause.
The
consequence of aerophagia is usually belching, also known as burping or
eructation. In the act of belching, the glottis is closed and the diaphragmatic
and thoracic muscles contract when the increased intraabdominal pressure
transmitted to the stomach is sufficient to overcome the resistance of the
cardia and the physiologic lower esophageal sphincter; the swallowed air is
expelled via a burp. Belching can become a chronic disorder with habit-forming
potential.
Belching
occurs from the beginning of life and is frequently seen in infants, who often
swallow air while drinking milk. In adults, belching may occur because of
overdistention of the stomach after a large meal. Certain foods such as
broccoli, beans, cauliflower, and other high-fiber foods can predispose to gas
formation and, in turn, belching. Food substitutes and medications that are
poorly digested may lead to gas and burping. Examples include sorbitol, which
is used frequently as a sugar substitute, and lactulose, which is used in
patients with constipation or hepatic encephalopathy. Inflammation of the
stomach from disorders such as gastritis or peptic ulcer disease can also lead
to stomach discomfort and the need to belch. Lastly, transient lower esophageal
sphincter relaxations that occur spontaneously while a person is upright and
awake can lead to the release of air from the stomach.
The
diagnosis of aerophagia is often made by careful history taking. Repetitive
belching can also be diagnosed by the history, although sophisticated tools
such as esophageal manometry, esophageal impedance, or impedance pH testing may
indicate that it is occurring. An increase in abdominal pressure coupled with
retrograde reflux and subsequent relaxation of the upper esophageal sphincter
signifies belching; other conditions, such as rumination, can also have these
signs, however.
Rarely
does aerophagia or belching lead to worrisome complications. The potential for
gastric volvulus, intestinal ileus, or perforation can theoretically exist with
excessive aerophagia, but they are rare and mainly seen in developmentally
disabled persons. These patients can be challenging because they may not be
able to follow recommendations. In these cases, other measures to
decompress the stomach or colon may be needed. Nasogastric, gastrostomy, or
rectal decompression tubes may be necessary to avert complications. More
commonly, aerophagia and belching are not at all dangerous, and the main
consequences are bothersome symptoms for the patient or his or her family.
Although patients often seek out medical advice for these troublesome symptoms,
they are often relieved to hear that neither condition is life threatening. The
best therapy for aerophagia and belching is education and behavioral modifications.
Investigations for pathologic conditions such as gastroesophageal reflux
disease (GERD) or peptic ulcer disease may be completed but are generally
unhelpful. For individuals who suffer from discomfort from aerophagia,
positional maneuvers can be helpful. Lying on the left lateral side or bringing
the knees up to the chest may help slowly release air without overt belching.
Although their effectiveness has not been proven, other treatment regimens
include reathing exercises, biofeedback therapy, and hypnosis.